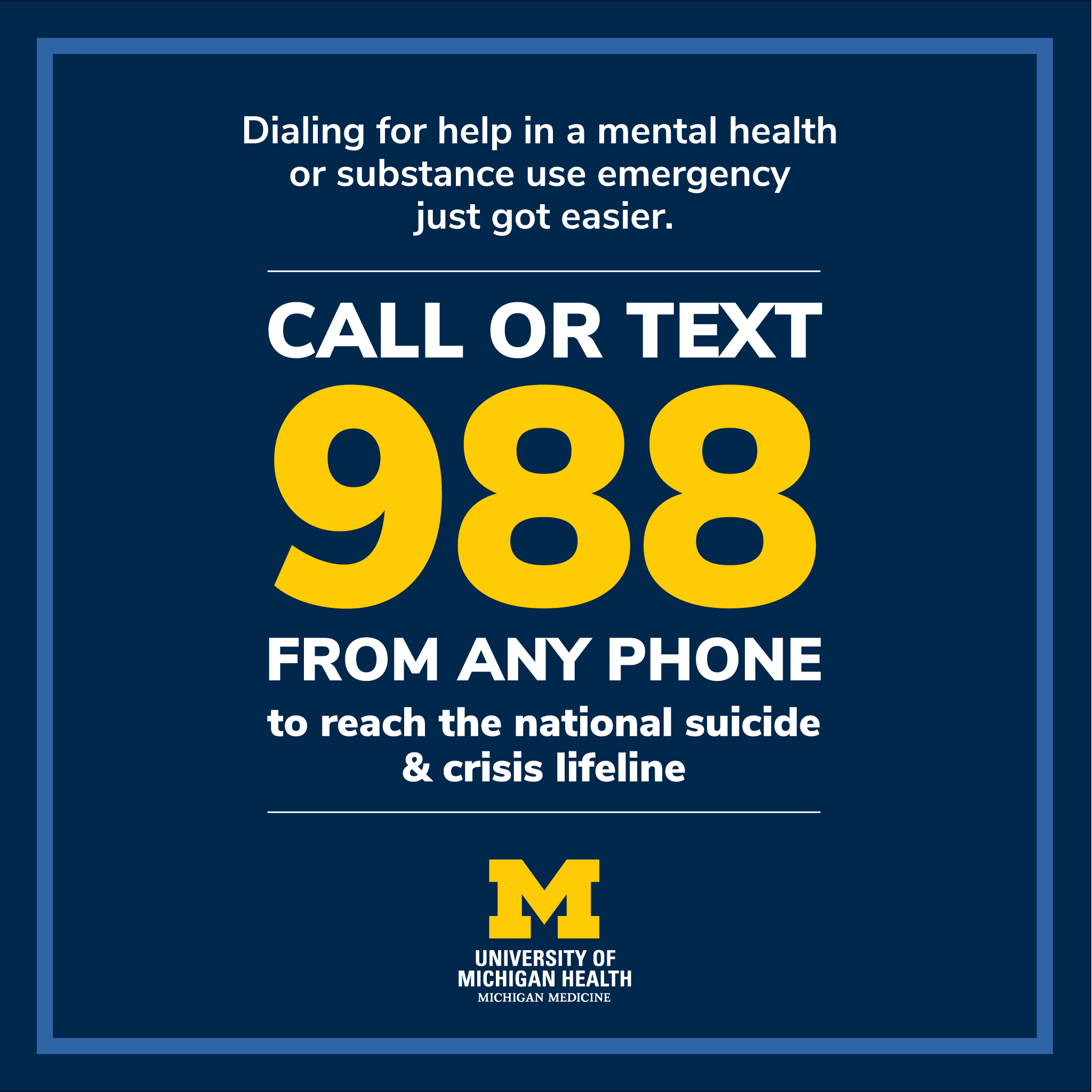
If you or someone you know is in immediate need of help for an eating disorder, or any mental health crisis, the national 988 Lifeline is the best place to start with. You can call or text 988 from any phone, or connect via webchat.
Recent studies, both nationally and at Michigan Medicine, have shown a sharp rise in the number of young people seeking care for eating disorders after the onset of the COVID-19 pandemic.
And it's a serious thing: these conditions are some of the deadliest mental health disorders to exist. Up to 20% of individuals with chronic anorexia die as a result of their illness, and, compared to the general population, individuals with bulimia nervosa are 7.5 times more likely to die by suicide, and those suffering from anorexia nervosa 31 times more likely.
Two experts from the Comprehensive Eating Disorders Program, a program based at University of Michigan Health C.S. Mott Children’s Hospital, and one expert from the Child and Adolescent Consult and Liaison Service, situated in the Michigan Medicine Department of Psychiatry, discuss the rise of eating disorders and what parents and others can do to help youth who may be at risk or showing signs of needing treatment.
An umbrella term
Christina Cwynar, DNP, CPNP-PC, a pediatric and psychiatric mental health nurse practitioner, explains that “eating disorders” is an umbrella term encompassing specific diagnoses that include:
- Anorexia nervosa
- Bulimia nervosa
- Binge-eating disorder, and
- Avoidant/restrictive food intake disorder
Although people may think of refusal to eat or skipping meals as the primary symptom, eating disorders also include:
- Emotional-behavioral symptoms, such as odd rituals, preoccupations with weight, food, or calories, social withdrawals, body checking, mood swings
- And physical symptoms, such as changes in weight, stomach cramping, constipation, irregular menses, difficulty concentrating, feeling cold, passing out, muscle weakness, poor wound healing, dental problems
Families, teachers, coaches and/or other loved ones may not directly observe an adolescent with an eating disorder restricting food, as it's very common for youth to hide this behavior, but they may instead pick up on these other symptoms first.
Cwynar says, during the pandemic, the loss of daily structure, pressures from social media, and/or food insecurity from paused of school meals were all common factors that caused adolescents to restrict their eating, with some habits eventually spiraling out of control.
Terrill Bravender, M.D., M.P.H., chief of Adolescent Medicine and the Rosen Professor of Adolescent Medicine in the Department of Pediatrics, adds that with the loss of extra-curricular activities, some adolescent athletes, fearing they would get out of shape for their sport, overcorrected by under eating or putting themselves on a harmful exercise regimen.
Misconceptions
Natalie Prohaska, M.D., medical director of the Comprehensive Eating Disorders Program, says the most common misconception that parents hold about that disease is that “eating disorders are a choice.” She emphasizes these disorders have multiple triggers and that, it is indeed, not a choice.
Another misconception is that “parents cause the eating disorder.” Parents are not the cause of eating disorders, and are instead, vital to curing their child’s illness.
Another is that individuals with eating disorders always appear emaciated or underweight, but Prohaska points out that this narrow view can prevent people who do not fit the assumed stereotype to receive the care they need.
Eating disorders affect individuals of all shapes and sizes, and it’s crucial to look beyond physical appearance when assessing the presence of an eating disorder. Further, although many people associate eating disorders with women, eating disorders are prevalent in men and transgender people as well.
“Eating disorders cross all barriers,” Prohaska said, who is also a clinical assistant professor in the Department of Psychiatry.
It's also a misconception that eating disorders will impact individuals for the rest of their lives. “Your adolescent can fully recover from their eating disorder and move on and have a full life ahead of them,” she said.
Resistance to treatment
Experts all agree it takes far too long for many young people with eating disorders to get diagnosed and treated.
Research shows that on average anorexia nervosa goes untreated for about 2.5 years while binge eating disorder goes untreated for about six. Yet, Cwynar emphasizes that people who get treatment earlier actually do better, with 60% of patients who seek professional treatment reaching a full recovery.
So, what should you do if you suspect your child has an eating disorder, but they’re resistant to treatment? Eating disorders can be difficult to treat since individuals often don’t want to get rid of their illness due to a distorted perception of themselves.
“As a parent, it is really important that if you are concerned about their medical health that you bring them in to their primary care provider,” she said. Although it is important to respect autonomy, the disorder prevents the child from thinking clearly or rationally. “As the parent, you have to step in and say, ‘we need to seek treatment’ because you can’t wait for the adolescent to be on board,” she added.
Treatment options
Prohaska emphasizes to families and patients that “food is your medicine.”
The malnutrition and behavioral components must be treated first to get the brain at a place where it can handle the talk therapy work. A lot of times families must involve professional help to help the individual eat more normally again.
The most evidence-based treatment for adolescents with eating disorders is Family-Based Treatment where parents or other caregivers help the child feed themselves to nourish their brain and body. Family is vital to the recovery of an adolescent because they know their child best, and the experts in the treatment team are there to support and empower parents through their child’s recovery.
More intensive treatment options include:
- Outpatient programs with multidisciplinary teams of practitioners
- Intensive outpatient programs that run a few days a week
- Partial hospitalization programs that run five days a week
- Residential treatment if the patient’s eating disorder cannot be managed in an outpatient setting
- And medical admission to a hospital if the patient needs urgent physical stabilization.
Bravender explains that health complications that can arise from malnutrition or self-induced vomiting can sometimes require an admission to the hospital and should always be assessed by a medical professional trained in eating disorders.
“There are numerous complications with malnutrition related to metabolic slowing,” he said. “A calorie is nothing but a unit of energy. If you’re not taking in enough energy, your body will do everything possible to conserve" it another way.
When the body is malnourished, intestines, heart rate, blood pressure, and even brain function, slows down. If individuals get back to a healthy weight as a teenager, there will not be long-term complications. However, if untreated, long-term complications to malnutrition include lost height growth for teens, lost menstrual functioning, hormone suppression, poor bone health, and poor dental health.
Prohaska says that treatments available now give adolescents with these disorders a fighting chance at making a full recovery.
“The eating disorder is something that will eventually be put in the past,” said Bravender, who remembers many patients who have recovered and are now able to reflect on the time when they were sick. “If you are worried, there’s the right help out there.”
Resources
- Find an eating disorders specialist or treatment program by visiting the National Alliance for Eating Disorders locator site or by calling their helpline, which is staffed by trained therapists, at 866-662-1235, Monday - Friday, from 9:00 am to 5:30 pm ET.
- Michigan Medicine experts recommend the website www.feast-ed.org as well as the National Alliance for Eating Disorders treatment locator and hotline
- Learn more about the Michigan Medicine Comprehensive Eating Disorders Program
- For additional information, visit the U-M Department of Psychiatry Mental Health Resource List