As a current resident in Pediatrics, Dr. Courtney Courter reflects on the valuable perspective she gained while navigating the transition from medical school to residency. In this episode, Dr. Courter discusses her personal journey with requesting accommodations, disclosing in her application, ranking residency programs, and ultimately finding the perfect match.
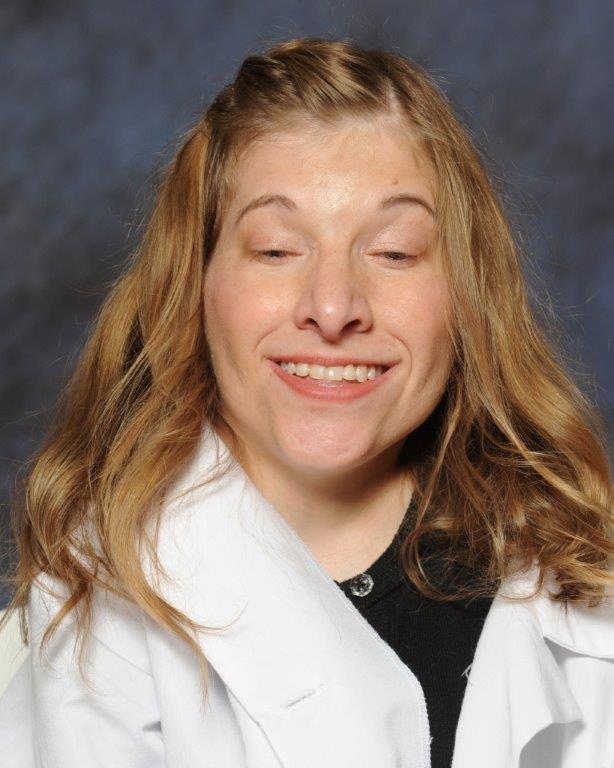
Courtney Courter, DO, Resident Physician-Pediatrics
Episode 14, Transcript
DocsWithDisabilities Podcast #14
Dr. Courtney Courter
Introduction: Lisa Meeks
Doctors with disabilities exist in small but measurable numbers. How did they navigate their journey? What were the challenges? What are the benefits to patients and to their peers? What can we learn from their experiences? My name is Lisa Meeks, and I am thrilled to bring you the Docs with Disabilities podcast.
Join me as I interview Docs, Nurses, Psychologists, OT’s, PT’s, Pharmacists, Dentists, and the list goes on. I’ll also be interviewing researchers and policy makers that ensure medicine remains an equal opportunity profession.
INTRODUCTION
Kate Panzer:
Welcome to the DocsWithDisabilities podcast. My name is Kate Panzer, and I am an MDisability research assistant at the University of Michigan Medical School. Today, we’re going to be talking about an important step in one’s medical career: the transition from medical school to residency. From residency applications to interviews to the long-awaited Match Day, the DocsWithDisabilities team wanted to explore these milestones further, from the perspective of learners with disabilities. Dr. Lisa Meeks speaks with Dr. Courtney Courter, a current resident who has successfully navigated this transition. Listen or read along as they discuss the topics of accommodations, disclosure, and how to choose a supportive and accommodating residency program.
Courtney Courier:
So I went to college at a school in New Jersey called Rowan. I studied biochem there, and then two years later I got accepted to medical school also at Rowan, which was wonderful. And then I applied to residency in pediatrics. So now I'm at a pediatric children's Hospital in Philadelphia. And I have a physical disability, it's called Arthrogryoposis Multiplex Congenita. So it affects my ability to walk. I can walk short distances, but typically I use a mobility device, usually a wheelchair, and then it affects all of my joints, like my wrists, my fingers, my knees. So things are a little bit harder for me, like bending my fingers and manipulating certain things. And then it affects my stature, so I'm very short. I stand at about four feet. It does affect my breathing a little bit because I have significant scoliosis, so I have to use breathing support at nights.
ACCOMMODATIONS
Kate Panzer:
Students with disabilities may need accommodations, which aim to even the playing field amongst their non-disabled peers. However, gaining access to these accommodations can often be an uphill battle for students in any academic setting. Dr. Courter openly shares the accommodations she requested in medical school, revealing how simple solutions can drastically improve a learner’s educational experience.
Courtney Courier:
Obviously there were a lot of barriers in applying to medical school. But my school was amazing, and they were super, super accommodating with me when I was accepted there. I think a lot of it was figuring out what I needed. I tried to be as on top of things as possible, but things definitely just kind of come up as you're doing something, you realize, oh, that's actually really hard. I think I'm going to need an accommodation here. In medical school, the big things that I needed were extra time on the physical exam when they would test you on that. I needed a lot of step stools. That was a big thing for me. Honestly didn't need too many.
I definitely struggled with getting appropriate time off for doctor's appointments. And I realized later that that was definitely an accommodation that I was entitled to but was really not always given. They would try to count it as a personal day, which we only had five of, or just say that I couldn't do it. So that was a really tough thing for me in trying to keep on top of my health. So when I was looking at residencies, that was something that I really took into account, whether or not they were going to be allowing me to see my own doctors when I needed to and that they really cared about your personal health and your wellness.
Lisa Meeks:
You really didn't need much, but would someone who is interviewing you for medical school have conceptualized that the accommodations that you needed were so minor? Or do you think they would have been concerned about additional barriers?
Courtney Courter:
Yeah, I think that they would be more concerned and that's kind of what I encountered throughout residency interviews too. Most people assumed that I couldn't do CPR or grilled me a little bit like, how are you going to suture and do CPR, which I did all of that, and that's always been a little frustrating because I don't have the option to not disclose my disability because it's so visible and apparent.
Lisa Meeks:
I think that so often we make assumptions about disability, right? I'm thinking of other students who are wheelchair users who could absolutely perform all of the clinical competencies and complete a performance checklist for everything from surgery to ObGyn. The point of this is: don't assume. I think in our society, people don't want to ask. They're afraid that they're going to say the wrong thing. How would you prefer that people approach your abilities and those particular competencies that would need accommodation?
Courtney Courter:
Asking is really just the best way to go. And my medical school, they definitely did ask me right away and wanted to know everything they could do to help. So they were very on top of it and were not afraid to ask. And I had the same experience once I started my residency. They've been super awesome, accommodating and always asking me, “How's it going? Is there anything else you need?” So I appreciate that so much.
I would say it was more of a challenge with residency interviews. They would dance around it or just ask me in a weird way. I had one interview where they said, “Wow, you can do so many things. What are you not going to be able to do?” That’s such a weird question. I guess it’s a different situation for interviews because you are afraid to disclose a little bit because you don't want to not be ranked because of it. But once you're accepted at a place, then you definitely hope that they will accommodate you at that point.
DISCLOSURE
Kate Panzer:
The transition from undergraduate to graduate medical education can be a thrilling yet daunting step in one’s career, particularly when an applicant is considering the disclosure of a disability. Drs. Meeks and Courter reflect on this process as they exchange tips and strategies to effectively disclose at various points in the residency application process.
Lisa Meeks:
Let's talk about this transition to GME. I see a lack of transparency, a lack of direction of who to contact. When do you disclose? Who do you disclose to? What are the procedures for requesting accommodations? How do you identify a program that will be a program that accommodates you? And I think our listeners especially are just hungry for this information.
For the most part, UME programs are amazing. They’re doing a great job of systematically processing student requests and understanding that disability inclusion is a wonderful form of diversity in that space. And I think for the most part, UME programs are working hard to get it right. I think in some way GME programs don't know what to do. Let's start with how you approached the match process.
Courtney Courter:
I knew that my disability was visible and so they were definitely going to know and likely going to ask me. And then when I went to my first interview, they asked right away. I felt like, okay, really need to come up with a solid plan because I kind of fumbled a little bit on some of what I said to them when they asked. I think I just sort of sat down and had a thought process with myself, ultimately decided to be very honest, and I think that went pretty well. There was always that level of fear, like when I said that, what was their reaction? Were they like, “Okay,” or were they like frivolously jotting down notes? And both of those things happened.
And then I always took notes after my interviews and wrote stuff down, like how did their reaction seem when you talked about accommodations? What was the facility like? That was a really big criteria when I ranked. Were there a lot of automatic doors? Was the call room super duper small or would I be able to get in there with my wheelchair? Were all of the computers very high and raised up? Would I ever be able to bring my wheelchair into the exam rooms?
Lisa Meeks:
Tell me how you situated your application. You said that you defined some talking points so that you could have very quick answers for the program if they asked. It sounds like you were being very proactive and as we both know it's illegal to ask certain questions in a residency interview. I think for somebody that has an apparent disability, you have to be the person that broaches the topic. Did you look at the board certification requirements for pediatrics and kind of work backwards thinking this will be what the program director and faculty want to know is can I meet these requirements, can I do these procedures? Or did you inform your talking points another way?
Courtney Courter:
That's a really good idea, and I probably should have done that, but I kind of just kept it a little bit more general and just talked about the big things like the CPR and PALS certifications and suturing. Pediatrics doesn't really have a surgery requirement but definitely procedural, and I actually really enjoy procedural. The way that I formulated my question about that was I would say, “Hey, I know that some residencies have a procedural elective. I really like procedures. Is that something that you would be willing to add to your program or think about allowing me to do as an elective?”
Lisa Meeks:
So it sounds like that was also your way of communicating to the program that you're capable of doing it. You took a more conversational approach, which was to inform them that you could do these by saying, “I really love doing these and I want to do more.” So that the perception would be, “Okay, well if she really loves doing them, by virtue of that logic, then she is able to do them.” How did you talk to your school about the MSPE and letters of recommendation for pediatrics? Were you involved in how your performance was communicated to the residency programs?
Courtney Courter:
In terms of them being able to talk about my disability, I was like, that's totally fine. When I wrote my personal statement, I wrote about it because as much as I want to be just Courtney and not have it all about that, it is a part of my story and it is a part of why I chose medicine and my experience with patients. So I did decide to talk about it in my application. So I gave my school permission to talk about it in their letters. I do believe that they added some of my feedback that I received on my ObGyn and surgical rotations where they talked about, “Courtney performed well with delivering babies and doing the typical ObGyn procedures.” So they did include that in my MSPE, and it was tactful of them to do that. If residency programs did have any question, it was written in my MSPE that I passed and did well on rotations that had procedural components.
CHOOSING A RESIDENCY PROGRAM
Kate Panzer:
When applying to residency, every applicant dreams of a supportive program that will prepare them to be competent and compassionate physicians. But how do you choose a program that will best fit your particular needs? We asked Dr. Courter how she evaluated and ultimately ranked potential residency programs.
Lisa Meeks:
How did you decide what programs you would apply to? Did you purposely look for institutions where people with disabilities had been successful?
Courtney Courter:
Yeah, I did. You apply to a lot of programs, so I wasn't as concerned about it when I submitted my 50 plus applications. But once I got my interviews, that was when I started to really research what kind of residents have they accepted in the past? The thing is, you don't always know just by looking at residents’ pictures or whatever that they're disabled. You might even find out later, they have an invisible disability, which I found out about my own program that there are lots of people with invisible disabilities, which is great cause they're kind of used to accommodating. There were two programs in particular that I did a rotation there. So I knew that they had had someone with a disability go through their program. So those programs in particular I did rank higher.
Lisa Meeks:
Do you think that there's something about having a resident with a disability that changes the culture of a residency program? Was there something unique in those residency programs that drew you to them? You said you liked the more.
Courtney Courter:
Yeah, so in terms of how the program directors and all the staff acted when I came to rotate there, they were like, “Oh my gosh, no problem. We can accommodate you.” For example, they got me a laptop to use cause I wasn't able to reach a lot of the computers that were up high on the tables where the nurses sit. So, they just gave me a laptop. They were like, “It's no problem. And anything else you need, don't hesitate to ask.” So that felt like such an easy fast accommodation. A lot of times too, people are willing to accommodate, but by the time the accommodation goes through, you're onto the next rotation. But they were like already set, ready to go, no problem. We can do that for you. We're already doing it for someone else. So that was great. And I think it made me feel like if I chose a program that had already had someone with a disability, I might be able to get the accommodations easier and faster and people would definitely be open to it.
I do think there's something cool in being a trailblazer though and being the first person at a program with a disability because you pave the way for the next people. So I wasn't afraid to be the first person at a program with a disability. For me, I just paid a lot of attention to how they reacted to me during my interviews and when accommodations did come up, did they seem open to it?
Lisa Meeks:
I know that you rotated in a few hospitals while you were still in medical school. Was that an effective strategy for programs that you thought you really might want to enter, to feel it out and be able to have access to information about the disability friendliness or disability responsiveness of a particular program?
Courtney Courter:
Yeah, absolutely. It was two fold for me. I mean your school tells you, if you love a place, definitely rotate there just to show your interest. So that was one part of it. And then exactly like you said, the other part was to kind of assess the facility while you were there. Like how accessible was it?
Lisa Meeks:
I wonder if your experiences having rotated at institutions or interviewed at institutions where they had successfully integrated a person with a physical disability and were really on top of it, if you used those programs as exemplars for an institution who had not done this, but where you were really interested in potentially matching. Did you ever say, “Hey, here's a list of five training programs who have successfully integrated students with physical disabilities? We could talk to their program directors if it makes you feel more comfortable.”
Courtney Courter:
I feel like that's a great idea. I never named specific institutions. The only thing I'd say that I did was I would say, “Hey, when I rotated during my fourth year, these rotations accommodated me really well and this is what they did for me. Do you think that you would also be able to do that for me?” I never really named institutions, but that probably could be a really good thing because then they might reach out to them and get more insight. So that's a great idea.
AFTER THE MATCH
Kate Panzer:
Fast forward to the excitement of Match Day, where students across the country finally discover both the specialty and institution where they will train for the next few years. For learners with disabilities, the previous conversations about disclosure and accommodations don’t end here. Let’s find out what steps Dr. Courter took to establish effective communication and understanding with her residency program.
Lisa Meeks:
Let's move to where a lot of people who are listening to this program are probably sitting right now. And that is, I've been accepted to a program, I've matched to that program. Now what? And this is of course for people that have known disabilities, there's probably been some level of conversation at this point, but for those that have non apparent disabilities, they might be deciding, you know, what do I do? Who do I contact? Tell us what you did when you matched, how you navigated and started that conversation.
Courtney Courter:
So maybe like a month or so after I matched, I reached out to the program directors and said, “Hey, I just want to, you know, be on top of everything and maybe we could have a conversation about accommodations I'm thinking at this point. And then she wrote back very quickly and we kind of just discussed over email. And then ultimately we set up a tour where the chief residents took me around to view the facility again so that I could see if there was anything else that I might need. My occupational therapist that I have who’s amazing at just finding really cool gadgets that are useful for me. She helps me attach things to my wheelchair so that I can carry extra gloves and things around. So she's just a great resource. They allowed me to bring her, and then they took me around and we viewed the call room and we were like, okay, that's not automatic. That's going to be tough. Let's put in a request for that. So it was just helpful to go to the facility too, cause the chiefs know where you’re going to be a lot and for them to show you what you're going to be expected to do, where you’ll be expected to be. And then I also looked at, for Peds there are cribs. How's the crib height? Does it go down at all, and will I need a step stool? And we measured the crib. How high is it? How high of a stepstool will we need? So going to the facility with the chiefs and my occupational therapist was very, very helpful for me in figuring out what I needed.
Lisa Meeks:
A lot of people talk about occupational therapists, and it's no surprise. I just think that they're the most creative people. But I haven't heard anyone say that OT was brought in to consult on potential accommodations in residency. I think it's brilliant, especially for programs that have an OT program. I think it shows a respect for other specialties and their nuanced knowledge and expertise.
Courtney Courter:
She was my occupational therapist through medical school too, so she's kind of seen me through the whole journey. So she was already very familiar with me, and she's just great. Within a day or two, she sent me links to like all these products. And then I work with an organization called Vocational Rehab. So I believe every state has some form of it. Essentially if your workplace isn’t going to provide the accommodation, Vocational Rehab sometimes picks up the cost of the accommodation. So like in medical school, Vocational Rehab did pay for one of my step stools, and they helped me get a ramp for my car. So that's how I found my occupational therapist through Vocational Rehab, and as long as I'm employed, I can still have that service.
Lisa Meeks:
Voc Rehab is super important because as you know, personal devices are not covered under the ADA. Institutions, so residency programs, medical schools, do not have to fund things that are considered personal devices, like a ramp to your car. But it is an essential necessity for you to get around and to be independent. I really encourage our listeners who may need a product, whether it be something that is designed for personal transportation or assistive technology that they get plugged into Voc Rehab. That's a really good recommendation.
So you matched. It sounds like you went through what we would call a robust interactive process. So there was a lot of you informing what you would need versus the program just saying yes or no. You're working hours that you've never imagined working, and there's less flexibility. But we had talked about your need for release for appointments in UME, and I'm wondering if you can speak to the audience about your continued need for medical appointments in GME and how that has been working.
Courtney Courter:
When I was looking at programs, that was something I considered as well. Whether or not they were all about resident wellness cause some programs had set protocols for that, which I thought was wonderful.
My current program is amazing with it. You just have to request it a little bit in advance, but you can take off a half day or if you need more than that, as long as they just know a little bit ahead of time so they can get someone to cover you. It's really no problem.
I’ve been extremely happy with my program so far. They’ve been wonderful. Not everybody has a visible disability, but I've just kind of learned as I've gotten to know people that they have these things and that they've been well accommodated.
ADVICE
Kate Panzer:
There is a lot we can learn from Dr. Courter’s recent transition from UME to GME. We were curious about the advice she would give to others who may also be considering a similar path to medicine.
Lisa Meeks:
What do you think are some major points that you would want to drive home for these listeners if they're thinking about disability in their programs or thinking about going into a program as a person with a disability?
Courtney Courter:
Yeah, so I would be honest and say that overall it's definitely more challenging and that's just kind of on a level of physical and emotional. Physically, I think that I do tire maybe more quickly than some of my able bodied co-residents or co-medical students. So I would say, it's gonna be hard and there are days you might doubt yourself for sure, but when you are properly accommodated and have that support, you can get through it. Keep at it and be open minded to different accommodations, different suggestions.
Even from your classmates. I would practice with my classmates, and they would come up with ideas like, “Hey, maybe if you just had a little more leverage you could do this.” And that was amazing for me that other people were being supportive and helping. Emotionally too, not just physically, but when you have a visible disability. I have always felt like I had to kind of prove myself when I would start a new rotation or even to patients and patients' families sometimes. They would kind of look at me or say something like, “You're a doctor. I don't understand.” And that can be like wearing on your confidence at times and a little bit emotional. And I even received a lot of that from residents, as a medical student when I would have residents teaching me and overseeing me. They would kind of doubt me. So that got definitely discouraging and emotional at times during medical school, but I was also very lucky to have a lot of family support and a lot of friendships that supported me through that. So I would just tell people that you're probably going to encounter things like that, but you know, keep your head up as best you can. Cause there are also amazing people and amazing teachers and amazing patients just as much as there are some of the discouraging ones.
Kate Panzer:
To Dr. Courter, thank you very much for taking the time to share your experiences and insight. And thank you all for reading and listening to this episode of DocsWithDisabilities. If you’ve enjoyed our podcast, please share it with colleagues, friends and family who may also learn from our content. We hope you join us next time as we meet with Dr. Cheri Blauwet, a sports medicine clinician and paralympic wheelchair racer.
This podcast is a production of the University of Michigan Medical School, Department of Family Medicine, MDisability initiative. The opinions expressed in this podcast do not necessarily reflect those of the University of Michigan Medical School. It is released under a creative commons, attribution noncommercial, nonderivative license. This podcast was produced by Lisa Meeks and Kate Panzer.
*This podcast was created using excerpts from the actual interview and is representative of the entire conversation. Interviewees are given the transcript prior to airing. Some edits may reflect grammatical and syntax adjustments for transcription purposes only.


