Adult Inpatient Rehabilitation: In September 2020, Michigan Medicine inpatient PM&R expanded services, opening a 24-bed inpatient rehabilitation unit at St. Joseph Mercy Chelsea (SJMC) Hospital. Michigan Medicine adult inpatient rehabilitation currently has 40 beds: 16 beds at University Hospitals (largely Cancer Rehabilitation and Spinal Cord Injury) and 24 at St. Joseph Mercy Chelsea (SJMC) Hospital (largely Neurological, Brain Injury and General Medical Rehabilitation). We are continuing to grow the Chelsea hospital rehabilitation center of excellence, and envision the remainder of adult inpatient rehabilitation, including cancer and spinal cord residency rotations, transitioning to Chelsea hospital, most likely during the 2024-2025 year. This move will unite adult inpatient rehab teams at one site, enabling residents and faculty to share teaching space, and it will provide us with a single, unified adult inpatient rehabilitation center of excellence.
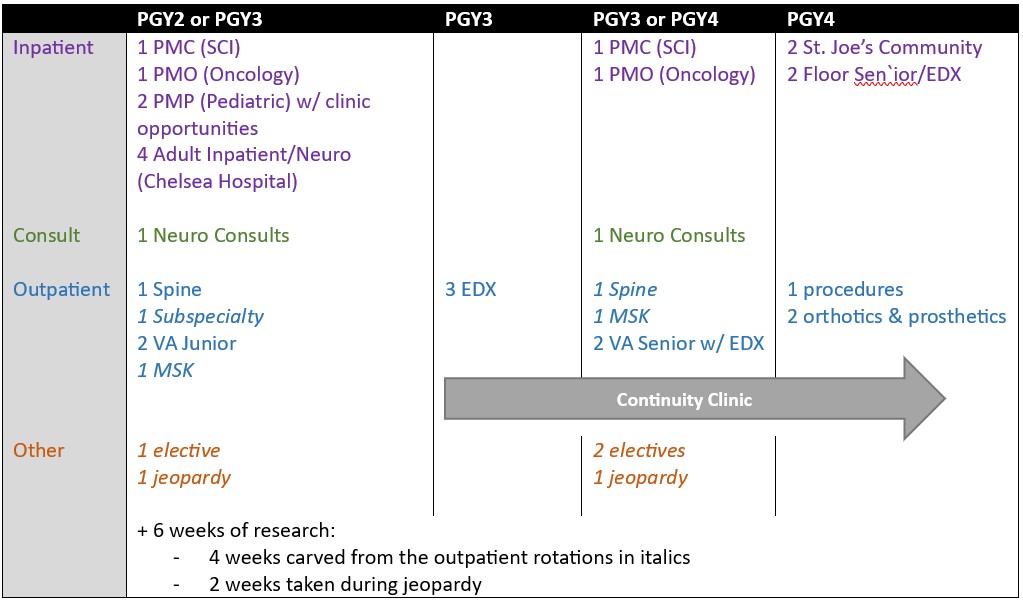
Our current rotations include:
- Adult Inpatient Rehabilitation at SJMC (Chelsea) Hospital (4 months): Neurological rehabilitation of patients with history of recent ischemic or hemorrhagic stroke or traumatic brain injury. Medical rehabilitation of critical illness myopathy/neuropathy, amputation, orthopedic trauma, acute immune-mediated neuropathies, and other complex conditions.
- Spinal Cord Injury Inpatient Rehabilitation at University Hospitals (PMC) (2 months): Residents will work mostly with patients with spinal cord injury from different causes including trauma, transverse myelitis, cancer, and ischemia. They will gain experience managing ventilator-dependent patients. Residents will also assist a spinal cord injury fellow or physician assistant with spinal cord consults.
- Cancer and Medically Complex Inpatient Rehabilitation at University Hospitals (PMO) (2 months): Residents will work with patients with functional deficits due to their diagnoses of cancer and/or other medical complexity. Some diagnoses residents will experience are supplementary motor area syndrome, radiation fibrosis, peripheral neuropathy and deconditioning due to chemotherapy. Residents will also gain experience in caring for recent bone marrow transplant recipients which will provide exposure to graft versus host disease, solid organ transplant, and those with complex needs (hemodialysis, intravenous immunoglobulin therapy, other infusables). Residents may get to work with cancer rehabilitation fellows during their two months on this rotation. During these two months resident will participate in M-CORE (mobile cancer rehabilitation team) rounds, twice weekly, and have special weekly didactic sessions dedicated to cancer rehabilitation with the cancer rehabilitation attending/fellow.
Pediatric Rehabilitation at C.S. Mott Children's Hospital (2 months): The resident will work under the supervision of a pediatric physiatrist attending and fellow. The resident will run the inpatient service and participate in inpatient consults.
Neurological Consults at University Hospitals (2 months): Consultation for management and disposition for patients under consideration for neurological rehabilitation.
Community Inpatient Rehabilitation at St. Joseph Medical Center (2 months): Two months are spent at St. Joseph Medical Center on the private rehabilitation service. This acute rehabilitation hospital has 30 beds. On this senior rotation, residents gain experience in a community hospital setting and work with physician assistants.
Senior Floor and Electrodiagnostic (EDX) Rotation (2 months): This Senior rotation develops skills for achieving independence in Electrodiagnostic Medicine and leadership, management and teaching skills on inpatient rehabilitation. Half of each day is spent as Floor Senior, adopting a leadership and teaching role and mentoring the junior residents on inpatient rehabilitation. Three half-days per week are spent in the EDX lab, developing advanced skills and discussing challenging cases.
Electrodiagnostic Medicine (EDX) (3 months): Initial training includes three continuous months (generally during the PGY3 year) of learning how to perform electromyography and nerve conduction studies. Time will be spent with both Neurology and PM&R EDX clinics. Overall, residents will get about six months of EDX training.
Musculoskeletal (2 months): This rotation will give exposure to the evaluation and management of common musculoskeletal problems, concussion management in athletes, participation in team clinics, and learning the basics of diagnostic ultrasound, ultrasound-guided injections, as well as tenex and other cutting edge procedures.
Orthotics and Prosthetics (2 months): Two months are spent on the Orthotics and Prosthetics service, which includes inpatient consults and outpatient clinics. (Wound care, lower extremity, upper extremity amputees, and adult and pediatric peripheral nerve injury clinics.)
Procedures (1 month): This senior rotation allows the resident to get more experience with specific procedures including baclofen pump refills, botolinum toxin injections, MSK procedures, and interventional spine procedures.
Spine (2 months): Two months are spent at the Spine Center, an outpatient facility dedicated to the prevention and comprehensive care of spine injuries with clinic days in our fluoroscopic-guided spine injection suite.
Subspecialty (1 month): During this rotation, the resident spends time in the rheumatology, spinal cord injury, and pediatric rehab clinics as well as multidisciplinary clinics including ALS clinic, cancer rehab clinic, Down Syndrome clinic, ventilator clinic, wheelchair seating, and wound care clinic
Veterans Affairs (4 months): Four months are spent at Ann Arbor VA Hospital through the course of the residency program. During the PGY-2 and PGY-3 years, a total of two months are spent working in a variety of outpatient clinics including musculoskeletal, orthotics and prosthetics, spinal cord injury, spasticity and pain management. During the PGY-4 year another two months are spent in same outpatient clinics as the clinics during PGY-2 and PGY-3 year with the addition of EMG as well as opportunities for Botox and ultrasound guided procedures. Overall, a large volume of musculoskeletal care and injection opportunities can be expected at the VA.
Resident Continuity Clinic: PGY-3 & 4 residents have their own continuity clinic one half day a week. This provides an invaluable opportunity to gain experience in seeing how disease processes mature while allowing residents to closely monitor the outcomes of the plans that they have put in place. This clinic also provides the resident with the opportunity to be a leading partner with the patient to help facilitate a patient's return to community/work/driving while navigating through the challenges that are presented to both the patient and the resident.
Elective (3 months): Residents build a clinical elective, seeking clinical experiences of their interest. There is also the opportunity to do an away elective during this time. Educational faculty leads offer recommendations on relevant clinical opportunities, and the program administrator assists in calendaring the electives.
Jeopardy (2 months*): The resident will cover other residents at the Inpatient Rehabilitation Facility, pediatric rehabilitation unit and consultative services when they take days off. During the times when the resident is not covering for a colleague, the time constitutes additional clinical elective.
Research (6 weeks): Six weeks of research are scheduled during outpatient and flexible rotations (see *rotations above); they are carved out in 1-week or 2-week blocks of protected time. The flexibility of scheduling affords residents the flexibility to invest in research projects at the times when project progress most demands it.