
Empowering Families as Leaders
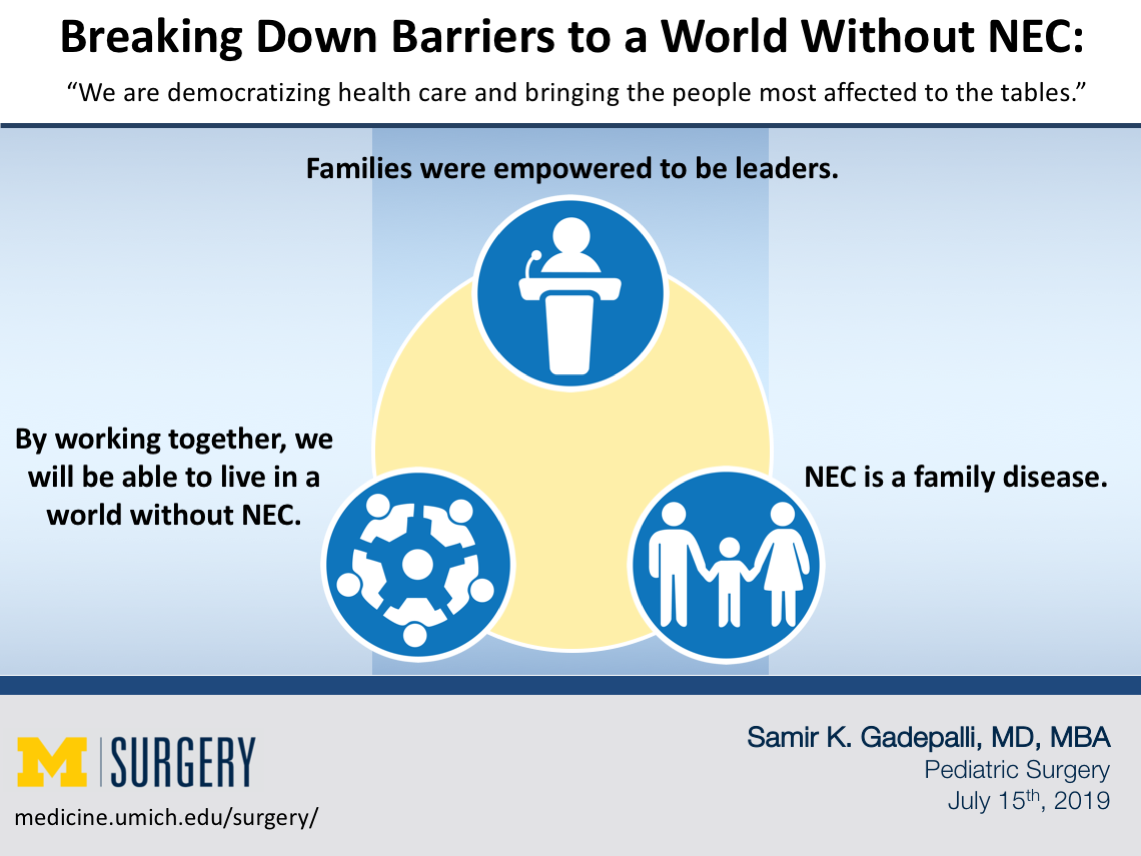
The current paradigm, whether in the Neonatal ICUs or at scientific meetings, is one where the families are only provided information as needed, lacking an ability to input into decision-making or voice ideas. There are several reasons for the current state, such as historically hierarchical systems, lack of education or awareness of neonatal disease in the general population, and time constraints. Patients and families had a voice during the 2019 NEC Symposium, and families were empowered to be leaders with involvement ranging from co-chairing the symposium to leading workshops and lectures. Though this seemed foreign initially during the conference, there was consensus by the end that this is how a meeting should be. The various groups were equally represented, and they were provided an opportunity to learn from each other.
Listening to Families Experiencing NEC
As a clinician, I have been part of countless meetings with families at the bedside, in clinic, in ICU settings, and emergency rooms. However, I failed to fully understand the daily life of a family who has been impacted by a disease for which they have never been prepared. After discharge, I see the families at my clinic and focus on the medical aspects of disease. The social aspects of disease become the burden of the family. Occasionally, we identify a cause such as the lack of funds for travel or the inability to skip work to come for an appointment, but these are relegated to the social workers in our system without the necessary resources to help families manage disease at home. A mother said to me as I prepared for the conference, “Do you know the sound a TPN machine makes at 3 in the morning? Do you know what it feels like to try to reset the pump when this is the only nutrition your child is receiving but it’s dark in the room and you don’t want to wake up your child?”
Before the conference, I thought I understood the essence of necrotizing enterocolitis (NEC). It is a disease that impacts vulnerable infants in a complex interplay between intestinal flora, inflammation, and a nutritional trigger with human milk having a protective effect. I realized how little I understood about diseases and the impact on families. NEC is a family disease. When you evaluate the common metrics such as hospital length of stay or need for ventilators, you miss the devastation it causes. The families are blindsided by the diagnosis, unable to clearly voice their choice in feeds, and live the rest of their lives with the results. They don’t get a chance to walk away.

Looking to the Future
We need to provide our families with the power to lead this fight against NEC. They have experience to understand the true nature of the problems that we as clinicians can never replicate. The lack of awareness is the first step for change that involves a common partnership, in which clinicians and researchers understand the pain the families endure and families are empowered with the knowledge and science to prevent and treat disease. As the impact is widespread, we will need to incorporate global perspectives from other countries, improve disparities in the care for families, and engage trainees and early career researchers. Funders will need to focus on promoting collaboration in research, inclusive of families – whether in basic and translational science, clinical trials, or quality improvement.
There is a need for urgency in better prevention and therapeutic regimens. The creation of a biorepository to collect clinically-linked biological samples during hospitalization should be complemented with long term patient follow-up and assessment of family quality of life measures inclusive of caregivers and siblings. The need to have universal access to human milk, clinical trials to use probiotics, and bringing novel therapeutic compounds to the bedside are priorities to decrease NEC rates. The use of quality improvement collaboratives such as the Vermont-Oxford Network (VON) can help standardize care and benchmark organizations. Every individual attending the 2019 NEC Symposium left with a responsibility to use the knowledge they gained during the conference. By working together, we will be able to live in a World Without NEC.
Article by Samir Gadepalli, MD, MBA
Downloads

