
Surgery & Research
My clinical practice as a reconstructive microsurgeon is integrally bound with my research program; they inform and enrich one another in fundamental ways. In my teaching both in the laboratory and the operating room, I remind my residents and medical students of the importance of understanding our own history as microsurgeons, and the significance of the early technical accomplishments of the pioneers that laid the foundation of clinical microsurgery through research. In the early days of microvascular surgery, Julius H. Jacobson performed the first microsurgical anastomosis of the carotid artery of a dog while using a microscope, and Harry Bunke conducted pioneering studies on microvascular free tissue transfer. Their work provided the basis of our modern microsurgical practice and also stimulated the minds and careers of those to follow: as both surgeons and scientists, their clinical practices formed the basis of their scientific pursuits. This core notion—that research and surgery are deeply interrelated—initially inspired and formed me and has continually guided my career. I have been fortunate at the University of Wisconsin to be in an enriched environment that facilitates both excellent clinical care and research, providing necessary protected time and excellent mentorship for both. I also strongly believe that both personal and professional growth is achieved through collaboration and interactions with those outside of our own university, particularly those with a rich history of excellent clinical care, research and education. The Department of Surgery at the University of Michigan is one such institution. Given UM’s outstanding culture and devotion to the three-arms of Academic Surgery, it was an honor to be the inaugural University of Wisconsin – University of Michigan Faculty Exchange Program Visiting Professor.
Why I Was Interested in Being the Exchange Visiting Professor to the University of Michigan
Basic Science
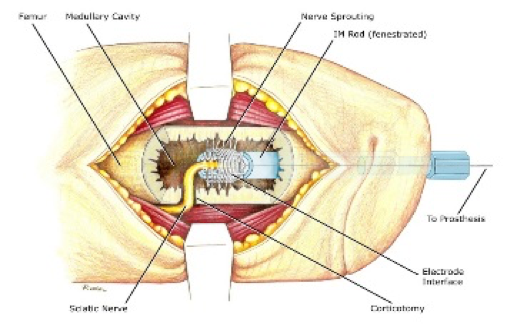
Figure 1 - Schematic of the Osseointegrated Neural Interface for Prosthetic Control.
The central focus of my federally-funded research program has been deeply influenced by my clinical practice as a reconstructive microsurgeon and my care of patients with peripheral nerve injury and amputation. Peripheral nerve injuries and extremity amputation have a tremendous impact on the public’s health; they include injuries sustained by civilians and veterans, and account for billions of dollars in health-care related costs per year. To address this critical problem, my research program is specifically focused on the peripheral nervous system and microsurgery, and spans two domains including the basic science of peripheral nerve regeneration and neural-interfacing for prosthetic control. The Section of Plastic Surgery at the University of Michigan is considered one of the meccas of peripheral nerve interfacing. The Michigan Neuromuscular Lab (under the direction of Dr. Paul Cederna) has developed the Regenerative Peripheral Nerve Interface (RPNI) which is a methodology designed to control advanced prosthetic devices. In early clinical trials, they have taken this technology into the clinical arena with good early success. Our lab’s invention – the Osseointegrated Neural Interface for Prosthetic Control – is another technology for prosthesis control and its invention was partly inspired by the work done by our colleagues at Michigan. I was inspired to be the exchange visitor to the University of Michigan to visit the Neuromuscular Lab to 1) learn more about their technology (first hand) and 2) to make headway in developing a future collaboration that would utilize both of our prosthetic control devices for improved clinical outcomes. The visiting professorship was incredibly fruitful. Not only did I spend several hours with Dr. Cederna discussing how to manage the constant battle between balancing research and clinical practice, I also met with several faculty who have been integral to the efforts in developing the RPNI as a viable clinical prosthetic control mechanism. Discussions were focused on efforts to develop the foundational basic science of the RPNI and the necessary steps taken towards clinical implementation and commercialization. This included one-on-one meetings with Drs. Cindy Chestek, Stephen Kemp, Theodore Kung and resident researcher (extraordinaire) Carrie Kubiak. In short, this visit was not only exceeding impactful to my own maturation into a balanced surgeon-scientist, but also provided the essential contacts for potential future collaboration as we move towards pushing the Osseointegrated Neural Interface into clinical translation.
Surgical Education
As academic surgeons, the greatest benefit the system affords us are the residents we interact with on a daily basis, the medical students seeking answers to questions that have fascinated them since their first day of Human Anatomy, and the undergraduate students seeking knowledge as they pursue a path towards their ultimate careers. I am constantly reminded through these interactions that education is one of our most important academic responsibilities, since it provides a direct connection to the next generation of clinicians, researchers, and thinkers. The University of Michigan Department of Surgery has the reputation for surgical education par excellence, and as the exchange professor, it was an honor to witness this process first-hand. I was able to attend resident teaching conference to observe Dr. David Brown expertly leading the group through multiple cases of facial reconstruction, I interacted with an excellent group of resident “research ambassadors” over tapas and iced tea, and had extensive discussions with Dr. Jennifer Waljee about surgical education and focused clinical practice informed by Health Sciences Research. I also had the opportunity to share my own thoughts on the ethics of radical body modification to a well-attended and attentive audience, as we discussed the “Morphological Basis of the Arm-to-Wing Transition.” I was so impressed with the ease of these interactions, the curiosity of the questions, and the depth of the thinking. It’s safe to say that surgical education is alive and well at the University of Michigan.
From Wisconsin to Michigan and Back Again: Bringing it Home
At the University of Wisconsin, we adhere to the Wisconsin Idea. This guiding fundamental philosophy, that campus activities should influence people’s lives beyond the boundaries of the university to the borders of the state and beyond, applies to all things we do including educational, scientific, and clinical advancements. After visiting The University of Michigan, I see clear parallels between the Michigan Promise and the Wisconsin Idea. The six missions defined by the Michigan Promise – Innovation, Recruitment, Leadership, Outreach, Environment and Achievement – provide the perfect framework to advance the Wisconsin Idea. So I returned home with a focused mission, informed by our colleagues at the University of Michigan, with a new view of collaboration, collegiality and the push for excellence across all domains. Go Blue (and Red).

Contact Us
Reach out to join the conversation or to learn more about how to implement the Michigan Promise. Connect with the Department of Surgery or our faculty on Twitter to share your ideas or get in touch with the Office of Faculty & Resident Life to schedule a Michigan Promise presentation at your institution. You can also fill out our Michigan Promise Inquiry Form with any questions or comments.
Department of Surgery
2210F Taubman Center
1500 E. Medical Center Dr.
Ann Arbor, MI 48109
Phone: 734-232-5528
Email: [email protected]
Twitter: @UMichSurgery
Hashtag: #MichiganPromise
