Over the past 7 years, we have built and sustained a faculty Leadership Development Program within our department of surgery. Each cycle includes approximately 25 faculty, and more recently, we have included 5-7 residents who are in their academic development time. We have recently completed the 4th cycle, ushering more than half of the faculty through the program. We have found this program to become a key tool for reflection on departmental challenges and opportunities; a unique opportunity to build relationships across clinical silos; and a launching point for other faculty development initiatives. We believe this program shows our commitment to relentless development of our faculty’s potential—and is central to the Michigan Promise.
In a series of blog posts, we will tell the story of how this program was developed and how it has evolved over time. We had many stumbling blocks along the way and changed many aspects of the program over the years. By telling this story, we hope to inspire others to pursue relentless faculty development; and to provide at least one path for building such a leadership development program, including a description of our struggles and blind ends.

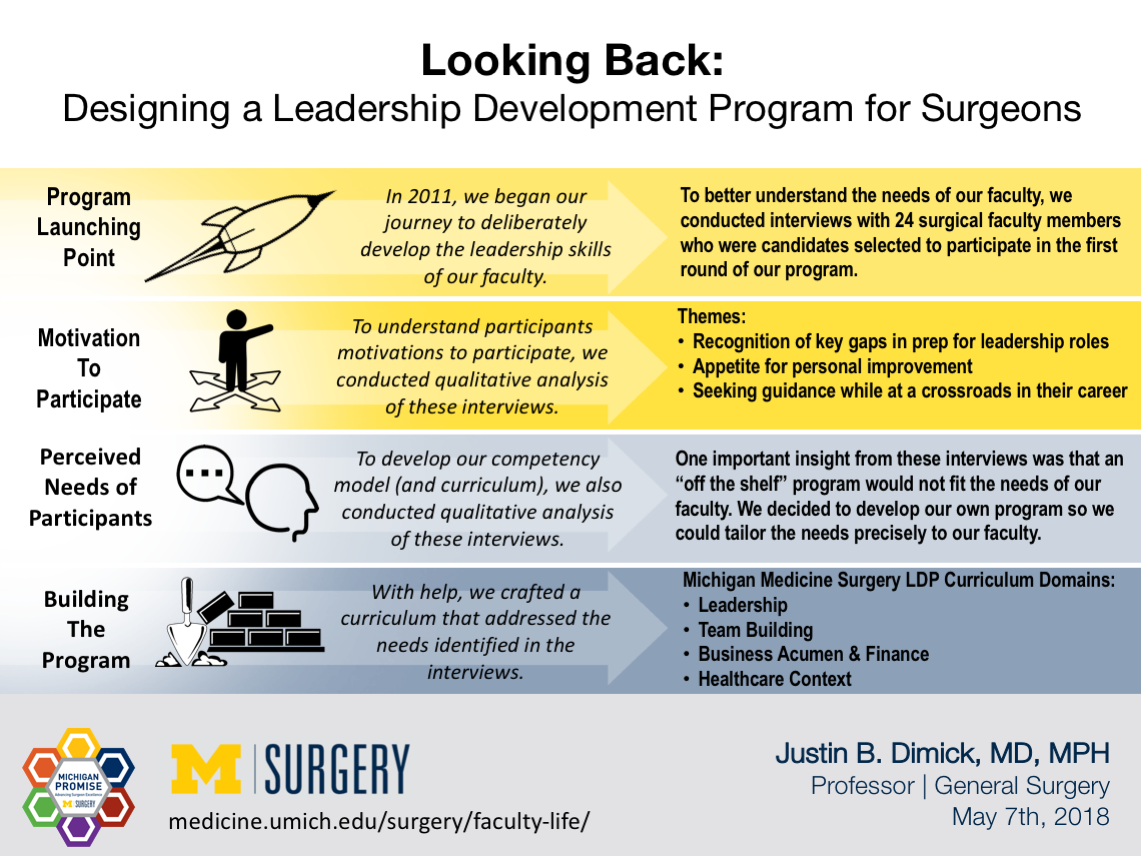
The Launching Point
In January 2011, at our annual department of surgery retreat, we began our journey to deliberately develop the leadership skills of our faculty. We believe that all surgical faculty are leaders in their daily life, whether conducting a complex procedure in the operating room, leading a division, or a chairing a committee in a national organization. But few faculty have had the opportunity to stop, reflect, and prepare for these opportunities. Surgical training is almost entirely focused on clinical care—developing technical skills and judgment—and appropriately so. However, we also recognized that we had an opportunity to prepare our faculty as leaders by addressing these gaps.
To better understand the needs of our faculty, we conducted interviews with 24 surgical faculty members who were candidates selected to participate in the first round of our program. We solicited voluntary participants for our program, including any faculty member who wanted to develop leadership skills, at any rank, from Assistant to full Professor. Most had an existing leadership role or were anticipating (or hoping for) new leadership roles. We were able to accept all applicants and only excluded a few new faculty (within 3 years of starting) as we thought these individuals should still be working on early career priorities—building a clinical practice, starting their research program, and learning how to teach residents and students. These individuals did participate in a future year of the program.
Motivation to Participate
To understand participants motivations to participate, we conducted qualitative analysis of these interviews (J Surg Res. 2016 Jan;200(1):53-58). These analyses demonstrated three key themes regarding faculty motivation to participate in a leadership program:
- Recognition of key gaps in preparation for leadership roles: Many participants were acutely aware that traditional medical school and residency training did not prepare them well for leadership roles.
- Appetite for personal improvement: Participants found themselves in leadership roles and are seeking opportunities to grow their skills.
- Seeking guidance while at a crossroads in their career: Participants found themselves at a point in their career where they must take on leadership responsibilities to continue to grow.
Perceived Needs of Participants
To inform development of our competency model (and curriculum), we also conducted qualitative analysis of these interviews. These analyses demonstrated four areas where we needed to focus our educational content:
- Leadership and communication: Learn effective communication and conflict resolution skills; and develop a compelling vision to motivate others.
- Team building: Learn to create collaborative, effective, diverse teams.
- Business acumen/finance: Learn about the basics of finance, marketing, strategy, and operations.
- Understanding health care context: Learn local context (e.g., organizational structure, and policies and procedures) and a greater understanding of health policy context.
These interviews were the basis for our competency model and guided us in developing the curriculum. One important insight from these interviews was that an “off the shelf” program would not fit the needs of our faculty. While there are many excellent leadership development programs offered through business schools, locally and nationally, we decided to develop our own program so we could tailor the needs precisely to our faculty. In particular, creating our own program allowed us to devote time substantial time in the curriculum discussing the local health care context, i.e., issues specific to our department and institution. To accomplish this goal, we incorporated health system and medical school leaders to discuss granular topics, such as strategic planning, financial statements, and how our institution is interfacing with national health care policies. We were also able to foster discussions with local leaders on what surgeons need to do to be active participants in health system strategy.
Building the Program
As the newly minted Associate Chair of Faculty Development charged with building this program, I knew I needed a lot of help. Luckily, help arrived in the form of Christy Lemak, PhD, Director of the Griffith Leadership Center, a highly regarded professor of leadership in the School of Public Health (now the Chair of Health Services Administration at University of Alabama Birmingham) and Robert Quinn, PhD who was a widely respected authority on leadership in the University of Michigan Ross School of Business. With the generous help of these individuals, and steadfast support from our Chair, Dr. Mulholland, we crafted a curriculum that was specifically tailored to the needs of our faculty discussed above.
Our initial leadership development program curriculum is shown below in Table. The program was 8 months long and included the following key elements:
- 8 full days of didactics: The backbone of the program was monthly Friday sessions where the entire group was present for didactics, experiential learning, and in-person group projects. Prior to enrolling, faculty had to clear their schedule and commit to attend all sessions, as we believed “dropping in and out” would disrupt the cohort effect. For each of the 8 days, we made it a priority to include high quality didactics, engaging speakers, and content that would be valuable to our cohort. As shown below, these days were designed to support learning in each of our areas of competency, including leadership, team building, business acumen, and healthcare context.
- 360-degree feedback and coaching: Each participant underwent a 360-degree evaluation by their direct reports, peers, and supervisors. The instrument was developed using questions from other validated sources that were combined to understand faculty performance according to our competency model. We also thought it was important to expose our faculty to executive coaching, as a tool for personal improvement. Each participant had two sessions with a coach to debrief and develop a personal improvement plan.
- Longitudinal group projects: To enhance team building among the cohort, participants conducted group projects during the program. There were a broad range of group projects conducted, but they all were aimed in some way to improve the department of surgery using what was learned during the program. As we will discuss in detail in later posts, many of the projects went on to launch new faculty development programs that are aimed to enhance faculty engagement and culture.
In our next blog post, we discuss the specifics of our curriculum below in more detail, including key design features, and our follow-up interviews with participants from our first cohort to understand what worked, and what didn’t.

Article by Justin B. Dimick, MD, MPH (Twitter: @jdimick1)

Justin B. Dimick, MD, MPH
Contact Us
Reach out to join the conversation or to learn more about how to implement the Michigan Promise. Connect with the Department of Surgery or our faculty on Twitter to share your ideas or get in touch with the Office of Faculty & Resident Life to schedule a Michigan Promise presentation at your institution. You can also fill out our Michigan Promise Inquiry Form with any questions or comments.
Department of Surgery
2210F Taubman Center
1500 E. Medical Center Dr.
Ann Arbor, MI 48109
Phone: 734-232-5528
Email: [email protected]
Twitter: @UMichSurgery
Hashtag: #MichiganPromise

