Dr. Donovan Maust received his B.S. in biology and international relations from the College of William & Mary in Virginia and earned his medical degree at the Johns Hopkins School of Medicine. He completed his psychiatry residency and geriatric psychiatry fellowship at the University of Pennsylvania before joining faculty at U-M in 2013. In 2019, Dr. Maust became Associate Director for Research of the Department of Psychiatry’s Geriatric Psychiatry Program, led by Dr. Susan Maixner. The Geriatric Psychiatry Program is one of the country’s largest academic geriatric psychiatry groups. In addition to his own research, Dr. Maust supports the ongoing work of Geriatric Psychiatry Program faculty as its members continue to grow and develop their work.
Dr. Maust is one of the few fellowship-trained geriatric psychiatrist health services researchers in the country — in other words, Dr. Maust is interested in understanding how care “in the real world” is delivered to older adults with cognitive or mental health problems, and what can be done to improve it. Dr. Maust’s “pet peeve” as a resident was seeing older adults who were on a large number of potentially inappropriate psychotropic medications, and understanding and reducing such prescribing has turned into one of his primary research and clinical interests. In addition, he is interested in how to better support family care partners as they help individuals living with dementia navigate the health care system.
With the support of collaborators in psychiatry and across the Medical School and university, Dr. Maust has several ongoing projects focused on older adults, which combine “big data” — such as Medicare claims from across the U.S. — with detailed interviews with patients and clinicians:
- With current support from the National Institute on Drug Abuse and the Centers for Disease Control and Prevention, Dr. Maust is leading work to help reduce harms of benzodiazepine prescribing (e.g., Xanax, Ativan) to older adults.
- A project supported by the National Institute on Aging is focused on reducing potentially inappropriate medical care that older adults living with dementia receive.
- A third project, supported by the U.S. Department of Veterans Affairs, is examining the VA’s remarkable success reducing benzodiazepine prescribing to older adults, which has not occurred for non-veteran older adults.
- His final ongoing project, funded by donor support, is investigating turnover and job satisfaction among direct care staff in long-term care facilities.
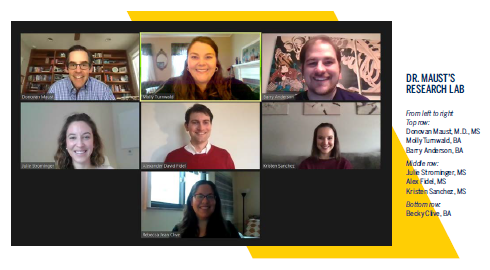
Fortunately, with help from the university’s IT support, Dr. Maust’s team quickly transitioned to remote work in the spring of 2020 and research activity has been able to continue relatively uninterrupted despite COVID–19. Dr. Maust has added a focus on the impact of COVID–19 to his work, including the projects on benzodiazepine prescribing and long-term care staff turnover.
Dr. Maust has continued to present his team’s work virtually, including at events for researchers (e.g., the Gerontological Society of America) and the general public (Michigan stop of the Alzheimer’s Foundation of America “Educating America” tour).