-
Ataxia Program -
Cognitive Disorders Program -
Comprehensive Epilepsy Program -
Health Services Research Program -
Movement Disorders Program -
Multiple Sclerosis & Clinical Neuroimmunology Research Program -
NeCTO Program -
Neuromuscular Diseases & ALS Program -
Neuro-Oncology Program -
NeuroSport -
Sleep Medicine Program -
Stroke Program

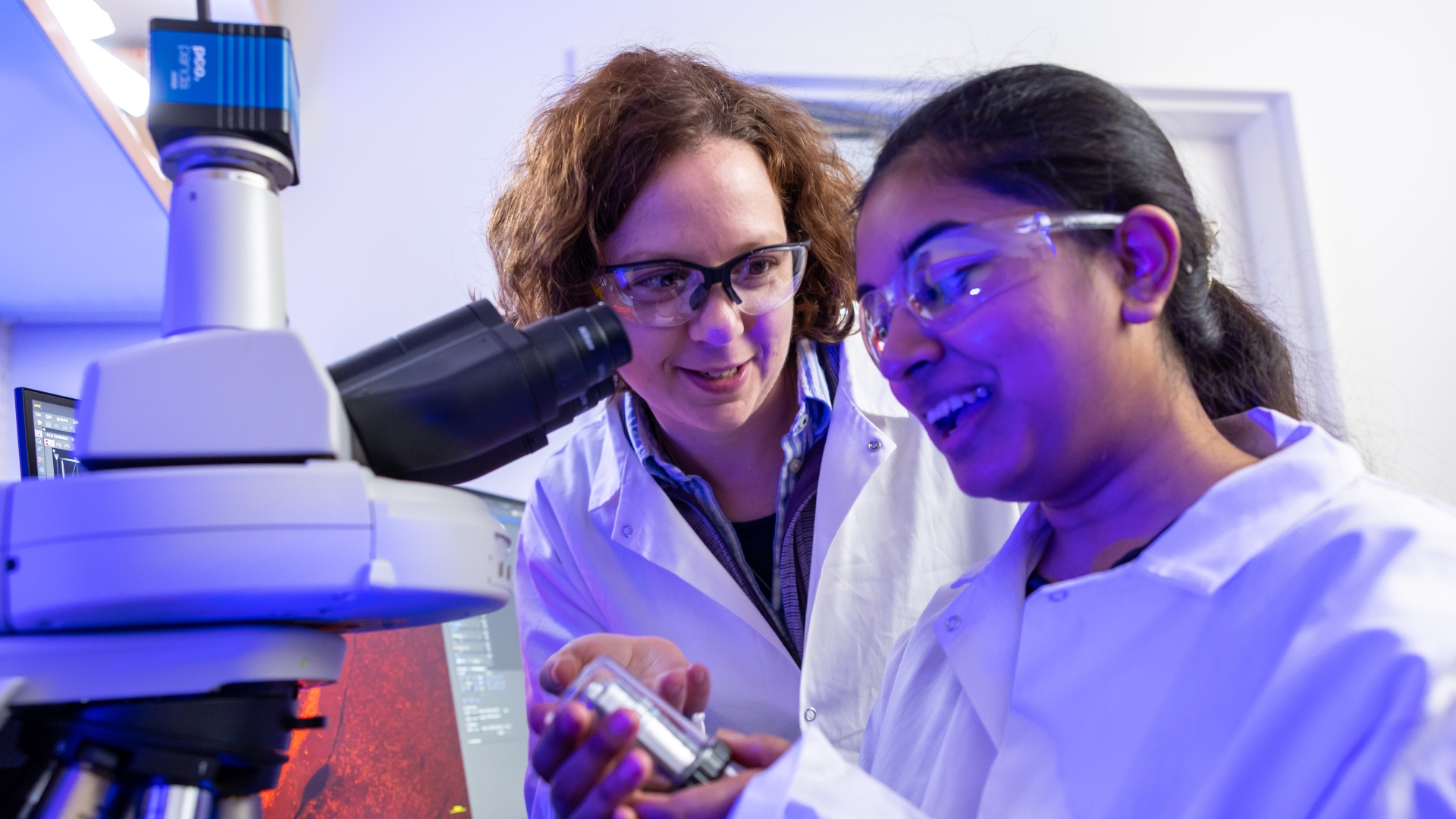
Explore & Expand the Science of Neurology
Delve deeper into disorders of the nervous system with world-renowned research programs changing what we know about these diseases and the lives of those affected.
The U-M Medical School Department of Neurology research programs span the spectrum of neurosciences. Explore basic studies in the pathogenesis of disease, the identification of conditions, patient-oriented disease phenotype studies, the response to novel treatments, epidemiology and health services research related to neurologic disease.
Learn more about our research strengths across all our divisions of Neurology science.
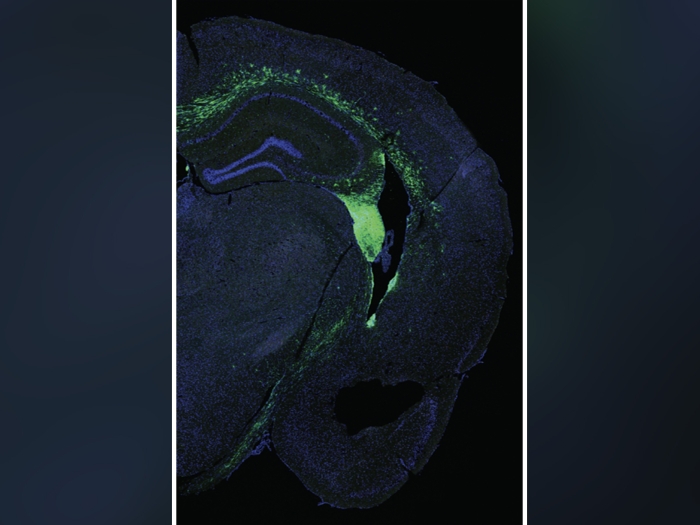
We are home to a multi-disciplinary campus-wide effort working toward a better understanding of, and an intervention for, Alzheimer's disease and related dementias.