As one of the first neurology departments in the country, we have provided generations of physicians and scientists with the knowledge, skills and compassion necessary to provide high-quality patient care.
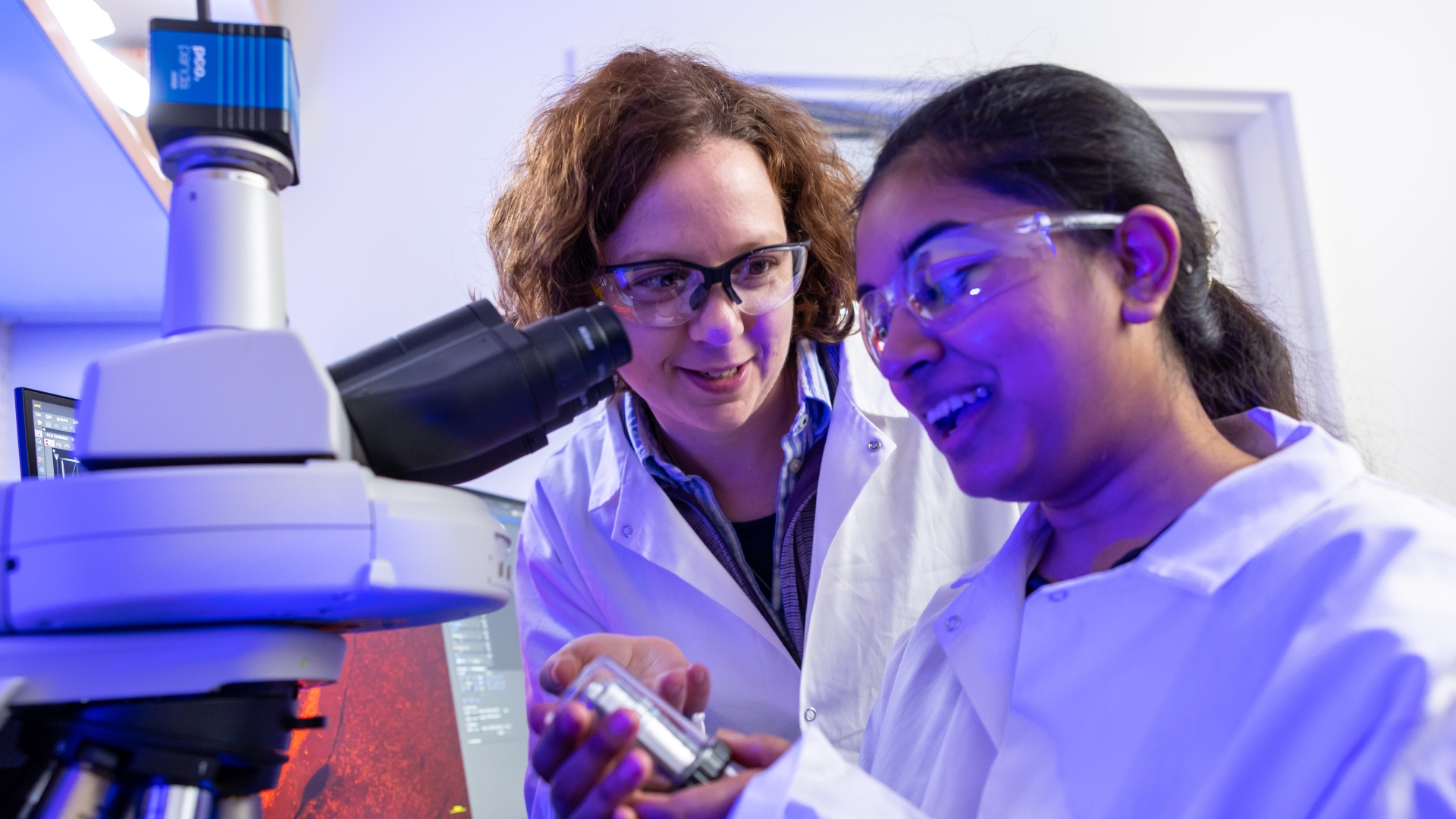
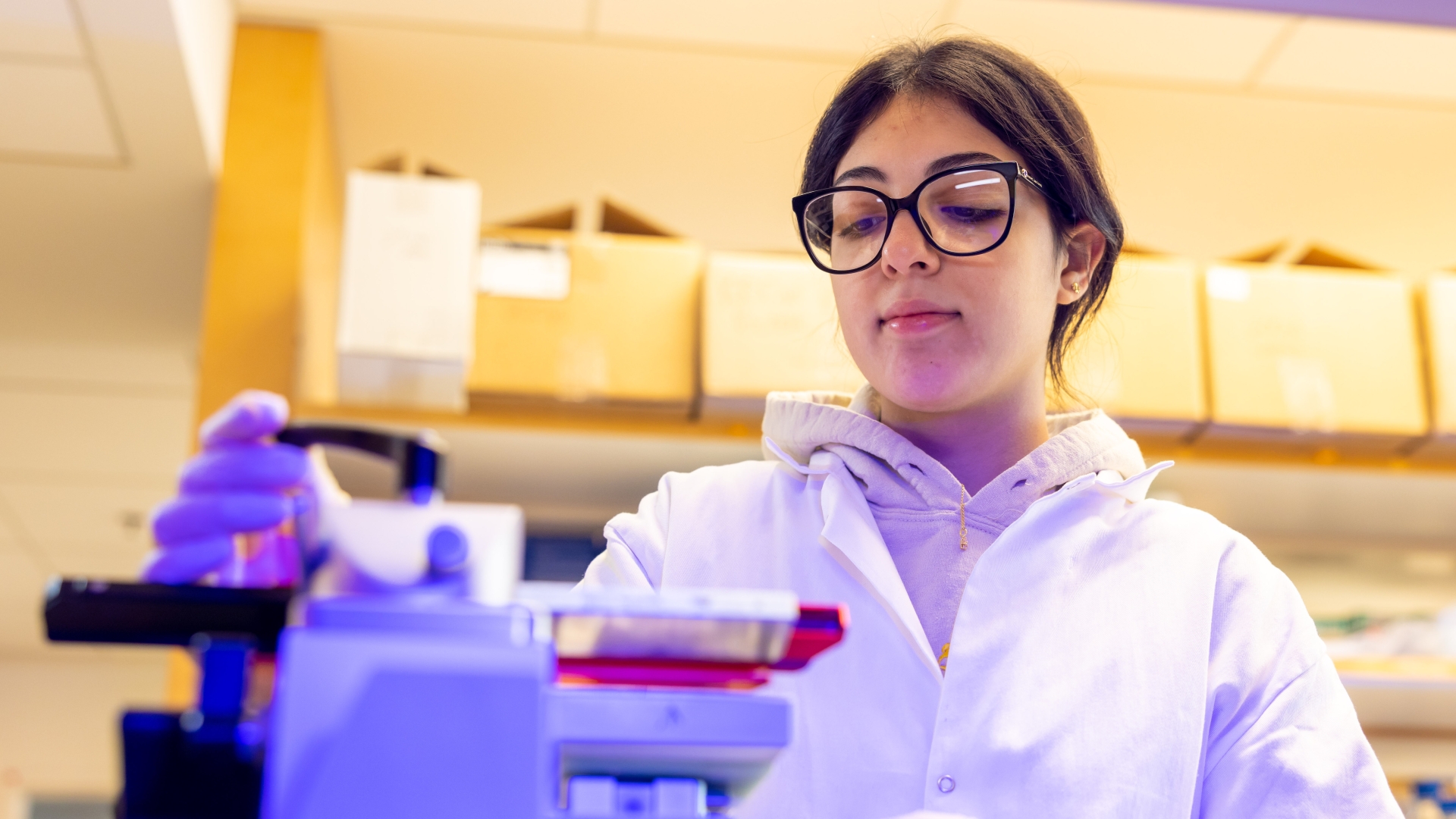
Our goal is to provide outstanding care for patients with disease affecting the nervous system, while also advancing our understanding and treatment of these conditions through research and other scholarly work. We believe we can better achieve this goal by fostering an environment that promotes health and wellness not only within the department but also across all segments of our community.

We are committed to promoting inclusion, diversity, and cultural sensitivity within our department and our community. To achieve this mission, we focus on five key areas: community outreach, underserved medical care, training and department engagement, recruitment and retention and communications.
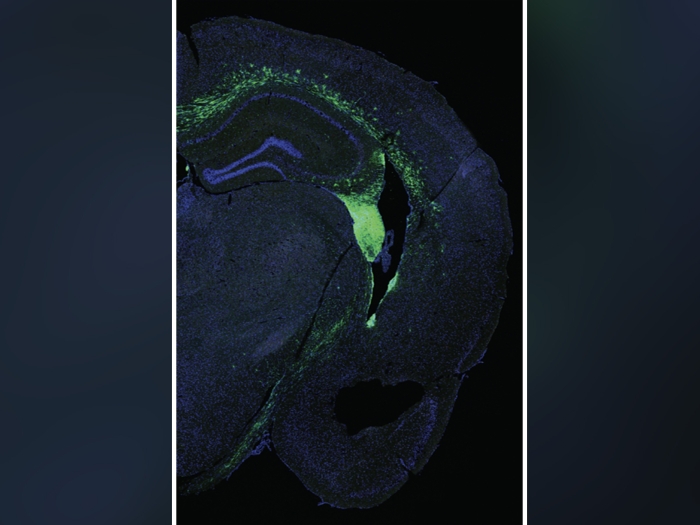
By supporting one of the nation’s leading neurology departments, your gift directly impacts patients and families facing debilitating diseases, such as Alzheimer’s, Parkinson’s and epilepsy.