Family Medicine faculty and residents will head to San Diego in droves, to attend the annual conference of the Society of Teachers of Family Medicine (STFM). Check out what U-M Family Medicine is bringing to STFM this year, with a number of exciting research and training presentations. A special thank you to all the faculty research mentors and family medicine staff for their support of resident-led research this year! Click on each presentation title to find details on the session, and follow the U-M Family Medicine Twitter account @UMFamilyMed for updates during #STFM50th!
Session Schedule
Friday, May 5, 2017
8:00 AM - 5:00 PM Coronado A
PR4 Leadership Development for New Faculty in Family Medicine: Learn New Skills in Mentorship, Scholarly Activity, Research Development, Advocacy, Wellness, and Resilience
New faculty face unique challenges navigating the multifaceted domains of medical student education, residency training, and research. Family medicine departments often struggle to provide a comprehensive orientation for new faculty or a sustainable model for continuous faculty development. Presenters will provide a toolkit for new faculty, providing guidance on faculty development, mentorship, coaching, giving effective feedback, scholarly activity, research development, advocacy, and faculty and resident wellness. Presenters will facilitate discussions on common challenges and fundamental resources including an updated toolkit incorporating feedback from annual sessions presented 2011–2016. A faculty panel will present leadership development activities, mentorship and coaching styles for seeking adequate support, take questions and offer advice including guidance on seeking and giving feedback, establishing an advocacy learning plan and agenda, research development, and creating an educator portfolio. A balanced approach to faculty life is becoming increasingly important with the increased administrative burden and limited wellness resources. Presenters will review wellness activities and modeling work-life balance.
Upon completion of this session, participants should be able to:
- Describe the most common personal, clinical, administrative, and academic challenges identified by new faculty in family medicine and identify resources for overcoming barriers.
- Identify effective mentoring and coaching concepts and styles, identify accessible opportunities for building mentoring and coaching relationships, and describe strategies for maintaining and modeling work-life balance.
- Implement faculty development programs, by learning about family medicine advocacy, faculty roles in supporting medical student interest in family medicine, and developing a pipeline of students and residents as new family medicine faculty.
Michelle Roett, M.D., M.P.H., F.A.A.F.P., C.P.E.; Rahmat Na'Allah, M.D., M.P.H.; Elise Morris, MD; Angela Kuznia, M.D., M.P.H.; Tyler Barreto, M.D.; Julie Petersen; Cheryl K. Seymour, M.D.
Saturday, May 6, 2017
7:15 - 8:15 AM Harbor Ballroom
B098 Create Your Own Adventure! How to Develop a Non-ACGME Accredited Fellowship Learning Experience
With the increasing amount of knowledge accumulating in medicine today, family medicine is in the business of creating life-long learners. Frequently, 3 years does not feel like enough time to acquire all the knowledge a family physician will need. Though family physicians are generalists at heart, individual residents often have a specific area of interest in which they wish to further develop skill. With the growth of Accreditation Council for Graduate Medical Education (ACGME) accredited fellowships such as sports medicine, adolescent medicine, geriatrics, and palliative care, there are more and more opportunities to expand the knowledge base. However, when a trainee’s area of interest falls outside of these few areas, how to acquire additional knowledge is more elusive. This seminar will share our experience at creating non-ACGME accredited fellowships in an area of individual residents’ choosing (community medicine and behavioral medicine). We will detail how we overcame the institutional and financial barriers, as well as success and outcomes, to help participants brainstorm similar programs within their own institutions.
Upon completion of this session, participants should be able to:
- Describe a model in which resident trainees apply and create a non-ACGME fellowship in an area of interest of their choosing.
- Articulate an approach to a financial model for a proposal for a non-ACGME fellowship.
- Articulate the pros and cons of developing a non-ACGME accredited self- directed fellowship and articulate the steps needed to create this within their individual setting.

Jill Schneiderhan, M.D.; Eric Skye, M.D.; Katherine Hughey, M.D.; Lydia U Lee M.D.; Margaret Riley, M.D.
1:15 PM - 2:15 PM Grand AB
P008 A One-on-one Model for Physicians Teaching Physicians More Efficient Use of Electronic Health Records
We will be showing that a one-on-one model using a physician to teach physicians how to better use electronic medical records (EMR) is effective and well received. Dissatisfaction among physicians with EMR, inefficient use of many of the helpful tools due to lack of interest, perceived time to learn, or understanding of how to access features all indicate the need for a more effective teaching method. Improved use of the EMR can lead to improved patient care, quality of care, physician satisfaction, and patient satisfaction. Our approach is unique in that it identifies gaps in knowledge or use of EMR tools, and then targets an individualized educational effort using a respected peer physician in a one-on-one setting, including observation during a clinic session with debriefing afterwards. Outcomes showed that physicians found the one-on-one sessions to be the most effective training method—it improved their job satisfaction, and it increased their ability to use the EMR. The fact that the teacher was a physician was very important to them. Productivity measures showed that participants decreased the time it took to close an office visit after training whereas nonparticipants time to close encounters markedly increased over the same time period.
Upon reviewing the poster, participants should be able to:
- Implement a one-on-one teaching strategy to help physicians increase their efficient use of EMRs.
- Use questionnaires to aid in planning a personalized curriculum as well as to evaluate the teaching.
- Use productivity metrics from the EHR as a proxy measure of evaluating teaching effectiveness.
Theresa Peters, M.D.; Grant Greenberg, M.D., M.A., M.H.S.A.; Timothy Guetterman, Ph.D.
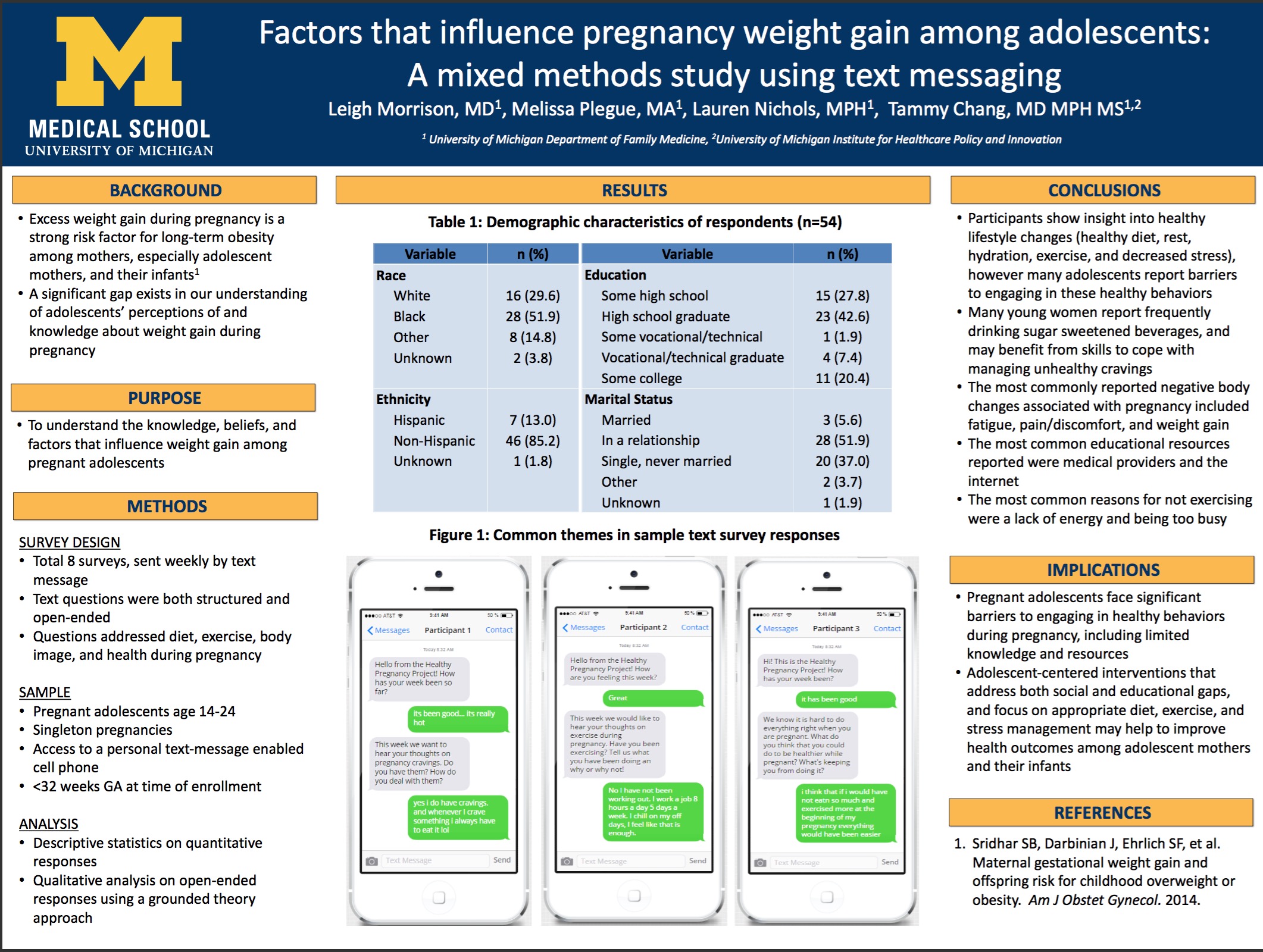
FP015 Factors that influence pregnancy weight gain among adolescents: A mixed methods study using text messaging
Excess weight gain during pregnancy is a strong risk-factor for long-term obesity among mothers and infants, especially among adolescent mothers. The objective of the study is to understand the knowledge, beliefs, and factors that influence weight gain among pregnant adolescents. In this mixed method study, pregnant adolescents age 14-24 with access to cell phones were asked a series of structured and open-ended questions using text messaging. The text message questions were sent after 20 weeks gestational age and focused on adolescents’ ideas regarding diet, exercise, body, image, and health during pregnancy. Descriptive statistics were performed on quantitative responses and open-ended text message responses will be qualitatively analyzed using a grounded theory approach to identify the knowledge, beliefs, and factors that influence weight gain among adolescents during pregnancy. Among our sample (n=54), the mean age was 21 (SD=2.2), with 52% identifying as Black or African American, 30% White, 13% multiracial, and 13% identified as Hispanic or Latino. Fifteen percent did not graduate from high school, 42% were high school graduates, 9% attended at least some vocational school, and 20% attended some college. In preliminary analysis of responses to date, three main findings have emerged. First, participants show insight into healthy lifestyle changes, including "cutting out candy", "do more exercising", and "not stressing so much." However, many women report barriers to engaging in these healthy behaviors ("No I have not been working out. I work a job 8 hours a day 5 days a week. I chill on my off days, I feel like that is enough"). The most common educational resources reported were the Internet, their physicians and midwives, and their mothers. Many young women also report frequently drinking sugar sweetened beverages ("I drink juice the most") and may benefit from skills to cope with managing unhealthy cravings ("Sometimes I have [cravings] and I deal with them by getting what I’m craving for" "I crave hot wings this week and I got hot wings"). Pregnant adolescents face significant barriers to engaging in healthy behaviors during pregnancy including limited knowledge and resources. Adolescent-centered interventions that address both social and educational gaps, and focus on appropriate diet, exercise, and stress management may help to improve health outcomes among adolescent mothers and their infants.
Leigh Morrison, M.D.; Melissa Plegue, M.A.; Lauren Nichols M.P.H.; Tammy Chang, M.D., M.P.H., M.S.
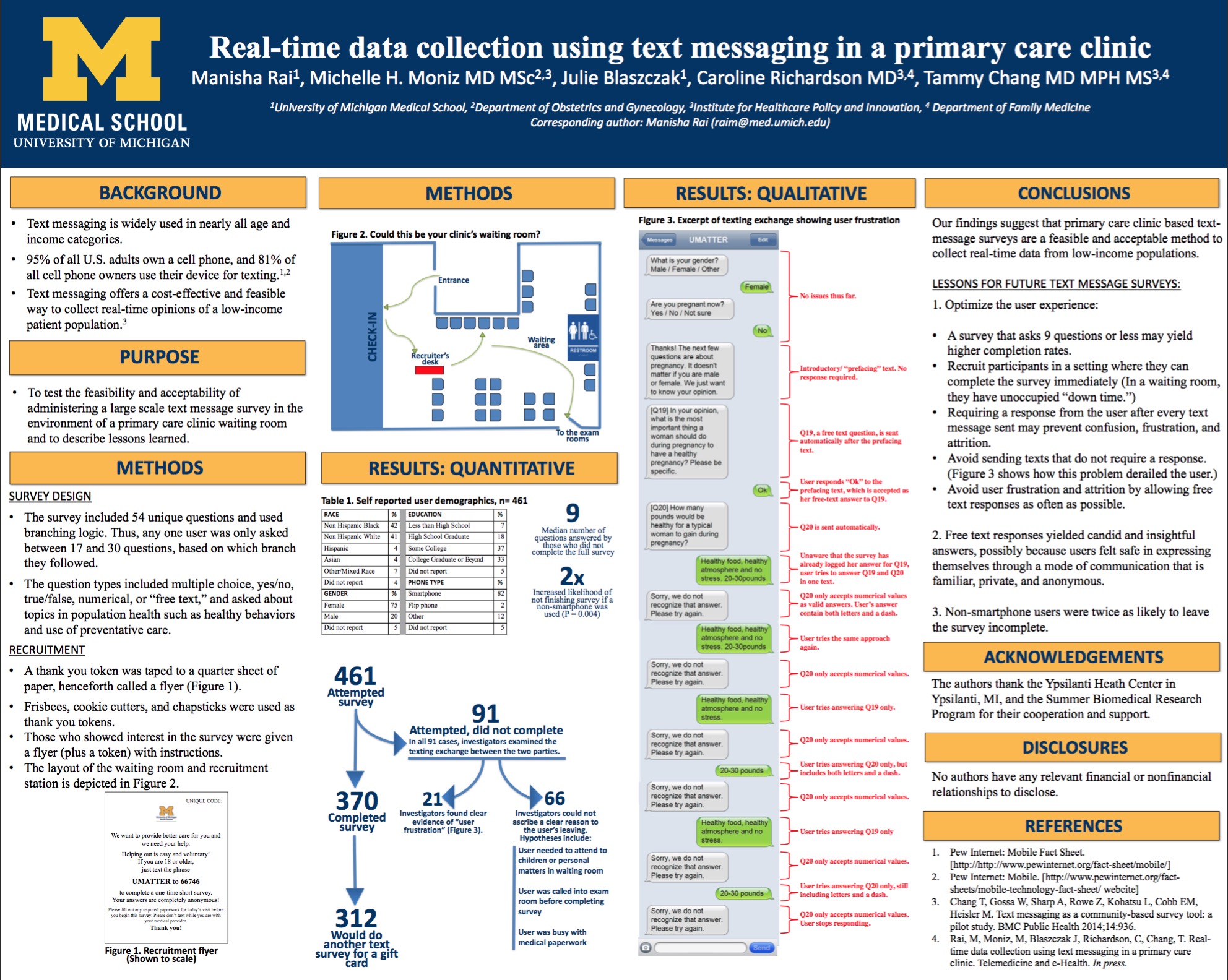
FP021 Real-time data collection using text messaging in a primary care clinic
Purpose: Surveys administered via text messaging may offer a convenient and cost-effective way for patients to "speak" to researchers in real-time about their health care knowledge, opinions, and beliefs. Our study aims to assess the feasibility and acceptability of administering a text message survey in the waiting room of a low-income primary care clinic. Methods: We obtained a convenience sample of individuals who entered the waiting room of a primary care clinic in a low-income community. All adults, including those who were accompanying patients to their appointments, were invited to join. Those that accepted the invitation to participate in the survey were given written and verbal instructions on how to begin the texting "conversation" on their cell phones. Survey questions included open ended and multiple choice questions. Descriptive statistics were used to characterize the participants and determine the response rates. Bivariate analyses were performed to identify predictors of incomplete surveys. Results: Of those accepting a flyer invitation, 43% (461/1061) attempted the survey. Of those who attempted it, 80% (370/461) completed it in full. The average age of respondents was 35.4 years (SD = 12.4). Respondents were predominantly non-Hispanic black (42%) or non-Hispanic white (41%), female (75%), and with at least some college education (70%). Of those who completed the survey, 84% (312/370) reported willingness to do another text message survey at a different time. Those with incomplete surveys answered a median of 9 questions before quitting. The majority of respondents (82%) reported using a smartphone. Smartphone users were less likely to leave the survey incomplete compared to non-smartphone users (15% vs 30%, respectively; P=0.004). Conclusions: Text message surveys are a promising modality for real-time data collection among low-income, clinic-based samples. Key lessons to maximize initiation and minimize attrition of text message surveys include a) offering a time for immediate completion of the survey (e.g. the waiting room of a clinic), b) minimizing the number of questions, c) simplifying the presentation of questions, and d) allowing "free text" responses for all question types, even multiple choice ones.
Manisha Rai; Julie Blaszczak, M.D.; Tammy Chang, M.D., M.P.H., M.S.; Michelle Moniz, M.D., M.Sc.; Caroline R. Richardson, M.D.
FP020 Testosterone deficiency, muscular weakness and multimorbidity in men: Not Just an Old Man’s Game
Purpose: The role of total testosterone (TT) production as a contributing factor for health and vitality in men is steeped in controversy. There is ongoing debate about what constitutes optimal physiological levels across different ages. Previous studies have shown a link between higher TT and protection against diabetes and cardiovascular disease, while other studies have reported no benefit. There is also a well-known link between TT and muscle strength in men, as well as between low muscle strength and chronic disease risk across populations. The purposes of this study were therefore to evaluate the independent and joint effects of TT and muscle strength on prevalent chronic multimorbidity in a population-representative sample of men. Methods: A population-representative sample of 2,399 men, aged 20 years old and older were included from the 2011-2012 National Health and Nutrition Examination Survey (NHANES). Prevalence of 9 chronic conditions was evaluated. Analysis were performed to examine the prevalence of multimobidity among young (20-39.9 years), middle-aged (40-59.9 years), and older (=60 years) men, with and without low TT. Multivariate logistic models were used to determine the association between age-specific TT tertiles and multimorbidity, adjusting for age categories and key sociodemographic variables. Results: Prevalence of low TT was 22.6%, 36.0%, and 34.9% for young, middle-aged, and older men, respectively. Multimorbidity was significantly more prevalent among men with low TT, compared to normal TT in the group (34.2% vs 50%; p<0.001); however, significant differences were only seen within the young (low TT: 33.3%; normal TT: 12.7%; p<0.001) and older men (low TT: 68.3%; normal TT: 57.3%; p<0.001). Fully adjusted models revealed an association between the age-specific low-TT (OR: 2.51; 95%CI 1.93-3.27) and moderate-TT (OR: 1.47; 95%CI 1.11-1.96) tertiles (reference high TT tertile) and multimorbidity. Mediation analysis demonstrated a mediation effect when NGS was included in the model, such that only low TT (OR: 1.78; 95%CI 1.20-2.64) was associated with multimorbidity. Conclusions: Low TT in men was independently associated with multimorbidity at all ages; however, multimorbidity was significantly more prevalent among young and older men with low TT. This provides evidence to support expanding testosterone testing to being considered as a screening test as a predictor of overall health.
Aleksandr Belakovskiy M.D.; Mark Peterson Ph.D.
FP006 Depression Screening in Pregnancy: Improving the Process
Purpose: Depression during the antenatal and postpartum period affects 3-15% of pregnant women and is associated with multiple maternal and neonatal morbidities such as pre-term birth, small for gestational age, decreased breastfeeding initiation and decreased antepartum clinic visits. This study aims to determine rates of depression screening during pregnancy to help implement quality improvement metrics. Methods: Study Design: Single-site cross-sectional study from June 2014-June 2016 at the University of Michigan. Setting/Intervention: 14 clinical practice sites including: obstetricians (maternal fetal medicine, resident run clinics, and attending only obstetricians), certified nurse midwives, and family medicine physicians. Dates of Edinburgh Postpartum Depression Screen (EPDS) completion, medical complications of the pregnancy, continuity provider and delivery group, and social work or psychiatry referrals were gathered from the EMR. Participants: 4,376 of 6,936 women who delivered between 6/2014 and 6/2016. Exclusion criteria: did not receive complete prenatal care at University of Michigan (prenatal, delivery, postpartum care), multiple fetuses, delivery prior to 36 weeks gestation. Measures/Main Outcomes: Data will be collected from the Epic EMR and analyzed for completion of EPDS surveys within each site and group for each trimester and post-partum screening. As a second component of the study, a survey will be distributed to providers at each site to gather opinions on current depression screening practices. Results: Initial results show that overall rates of depression screening vary from 9% to 57% depending on the trimester screening is provided and the continuity group. First trimester screening rates ranged from 37% to 48%. Post-partum screening ranged from 9% to 51%. Further data analysis is needed to verify results and identify which clinical groups and clinics are performing above average depression screening for the institution. Conclusions (anticipated): It is expected that EPDS screening rates will be highest in the 1st trimester due to an institutionalized work flow process that allow for screening to be offered regardless of provider or site. Initial data shows rates for screening at the post-partum visit are significantly below those at the 1st trimester visit. If this is verified with further analysis quality improvement measures will be determined to create the largest impact in depression screening in pregnancy.
Gwendolyn Fitz-Gerald, M.D.; Niyati B Shah, B.A.; Carrie Bell, M.D.
4:00 - 4:30 PM Golden Hill A
L020A Lessons Learned in Developing a Specialized, Non-clinical Curriculum for Medical Students
With increased emphasis on primary care and the social determinants of health, family medicine physicians are in a crucial position in today’s health care landscape. Likewise, family medicine educators are well positioned to lead change in medical education in these areas—though this can be a daunting task. How does a family medicine educator create an innovative, effective curriculum to engage learners in these important areas? At the University of Michigan, family medicine educators are leading curriculum development in specialized, non-clinical areas of focus for medical students. This lecture-discussion session aims to summarize the experience of family medicine faculty creating a global and domestic health disparities curriculum for second year medical students. Key, generalizable features of successful curricula will be reviewed, including characteristics of adult learners, evidence-based hallmarks of effective curricula in medical education, and techniques for actively engaging learners in relevant material. Participants are encouraged to share lessons learned and best practices in the development of similar curricula in their home programs.
Upon completion of this session, participants should be able to:
- List four techniques to actively engage adult learners in a teaching session.
- Identify three characteristics unique to adult learners as a target audience for education efforts.
- Apply lessons learned in curriculum development to their own educational endeavors.
Saturday, May 6, 2017
2:30 PM - 3:30 PM Ocean Beach
S11 A FRESH Approach to Difficult Conversations on Race, Ethnicity, Religion, Sex, and Culture
Family medicine physicians care for diverse population and recent events in the media, such as police shootings of civilians and the Syrian refugee crisis, affect us emotionally. The Detroit Medical Center/Wayne State University Family Medicine Residency has developed a structured tool to facilitate conversations on topics that are potentially difficult to discuss, such as race, gender, sex, culture, and religion. This tool, the FRESH-CC (Framework for Racial, Economic, Social/Sexual, and Humane Cultural Conversation) provides a processing method for use with any teaching technique, such as book club, didactic lecture, field experience, or longitudinal curriculum. The FRESH-CC starts with identifying the subject matter to be discussed, followed by a survey of the learner’s attitudes and comfort with the material. Using this survey, a facilitator can use different techniques (i.e. write-pair-share, small group discussion) to help group members discuss potentially difficult topics. Our seminar will introduce this FRESH-CC tool through an interactive session where participants will use the tool to discuss an article addressing a controversial topic, and we will share preliminary data of our experience using the FRESH-CC.
Upon completion of this session, participants should be able to:
- Define the key components of the FRESH-CC that provide a structured intervention in facilitating discussions among family medicine learners.
- Use the FRESH-CC to facilitate a difficult discussion among a diverse group of family medicine learners.
- Identify opportunities in their family medicine curriculum where the FRESH-CC can be used to foster more effective communication on important but difficult conversations.

Stephen Warnick Jr, M.D.; Randal Harris; Maricela Castillo MacKenzie; Erin Hendriks, M.D.; Fatin Sahhar
4:30 PM - 5:00 PM Golden Hill A
L020B Transforming Preclinical Student Experiences Through Adolescent Health Education: The Story of MiHealth
Universal, high-quality health education for adolescents is lacking, especially in underserved communities. Maximizing the interactive nature of curriculum and utilizing presenters who are not traditional classroom teachers can improve health education outcomes. Additionally, medical students’ empathy has been reported to wane during medical school, yet community involvement seems to be a protective factor. In this session, we’ll tell the story of what happened when preclinical students set out to improve adolescent health outcomes at a local, at-risk high school. We will share experience, data, and insight gained through our first two years of MiHealth, an intervention that brings medical students into the classroom to tackle critical topics like sexual health, mental health, and substance abuse. This session will engage in a deeper dive into how student-led organizations can start out with a strong foundation, use data to continuously improve, and establish a sustainable framework to make a long-term impact. We will ponder cost-benefit of programs like MiHealth, discuss common challenges, and share ideas and lessons learned from any similar programs from their home institutions.
Upon completion of this session, participants should be able to:
- Identify potential needs, stakeholders, and anticipated challenges involved in starting an intervention to address community health.
- Reflect upon approaches to curriculum design and outcomes for medical student educators and leaders as well as learners in the community.
- Consider the variety of tools used in program evaluation and discuss ways to increase the utility of data collected, while anticipating common limitations and constraints.
Margaret Riley, M.D.; Kate Meixner; Kate Brown
Sunday, May 7, 2017
10:00 AM - 11:00 AM Grand AB
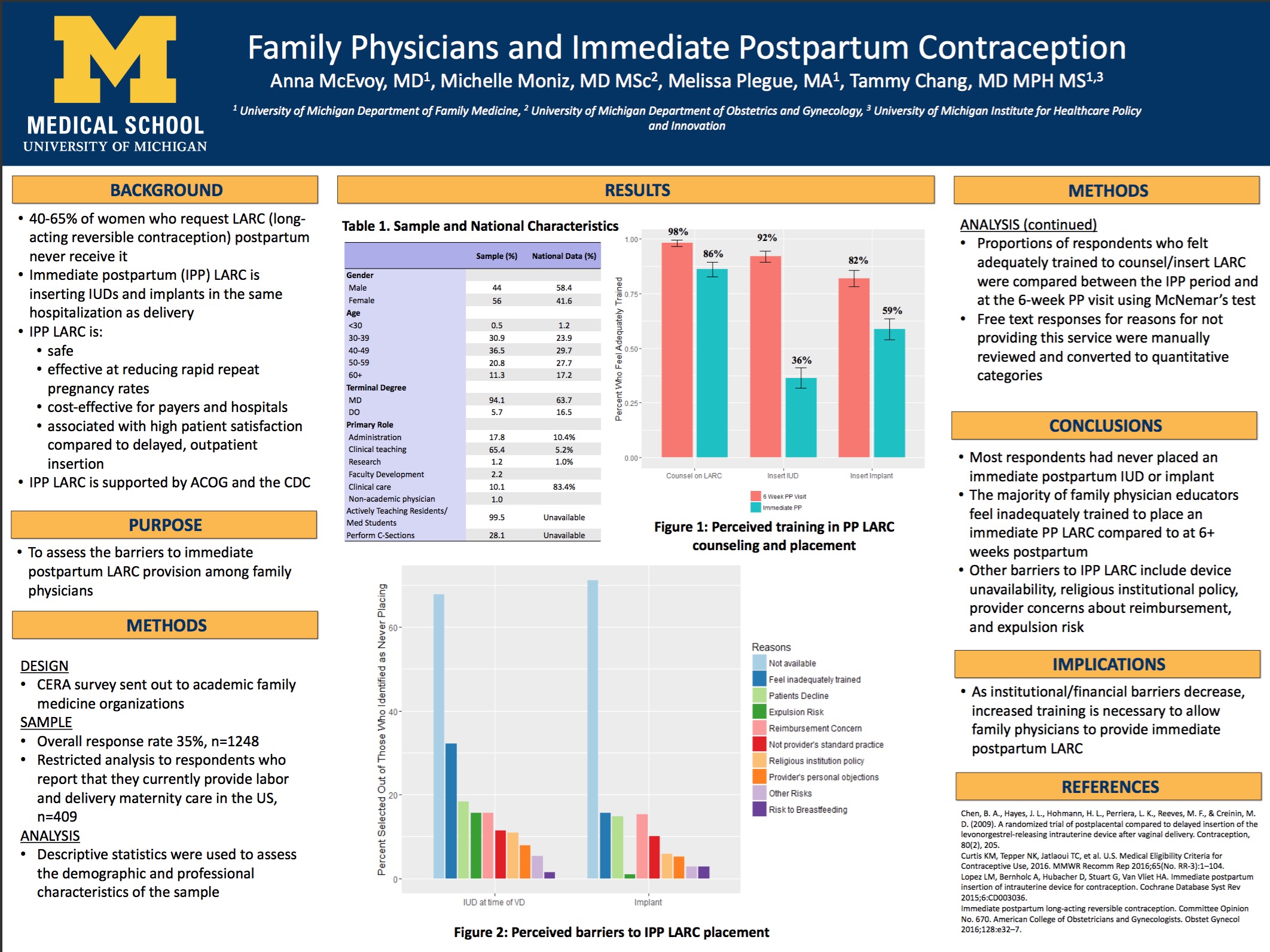
RP35 Family Physicians and Provision of Immediate Postpartum Contraception
Family medicine physicians play a substantial role in providing perinatal and contraceptive care. Immediate postpartum long-acting reversible contraception (IPLARC), or inserting IUDs and implants during the same hospitalization as delivery, is a promising strategy to help women with poor access to postpartum care achieve their family planning goals. There is a robust body of evidence that shows IPLARC to be a safe and cost-effective option. Despite this evidence, there are multiple barriers that may impede access to IPLARC, both at the institutional and provider levels. This study assessed current family physicians’ level of knowledge, experience, and barriers to offering IPLARC.
Upon review of this poster, participants should be able to:
- Define immediate postpartum long-acting reversible contraception.
- Explain perceived barriers to immediate postpartum long-acting reversible contraception.
- Apply knowledge gained regarding barriers to immediate postpartum long-acting reversible contraception to advocate for increased availability and training at participants’ home institutions.
Anna McEvoy, M.D.; Michelle Hofmeister, M.D.; Tammy Chang, M.D., M.P.H., M.S.; Melissa Plegue, M.A.; Michelle Moniz, M.D., M.Sc.
FP063 Multifaceted wellness curriculum to reduce depression, anxiety and burnout rates among first year family medicine residents
Purpose: Burnout affects nearly half of practicing physicians in the United States and a number of studies have suggested that physicians in-training are at particularly high risk. Our study seeks to evaluate the impact of a longitudinal wellness curriculum aimed at promoting self-compassion and mindful awareness on reducing rates of depression, anxiety and burnout among first-year family medicine residents. Methods: Study design: Longitudinal wellness curriculum composed of three 4-hour sessions over one academic year. Participants: 11 first year residents in the intervention group and 20 second and third year residents in the control group. Measures/main outcomes: Sessions cover the following skills-based topics: Mindfulness, self-compassion, mindfulness-based cognitive behavioral therapy (MBCT), and acceptance and commitment therapy (ACT). Confidential online surveys using validated questions from the Patient Health Questionnaire-9, Generalized Anxiety 7-Item Scale, Mindful Attention Awareness Scale, Self-Compassion Scale, and the Maslach Burnout Inventory will be used to assess baseline scores and changes over time in response to the intervention. Descriptive and correlational statistical analyses will be conducted on the survey data to determine significance. Results: Data and results are not yet available as our study is currently in-progress. We have completed the first of our three-part intervention and are preparing to hold our second session in February 2017. Conclusions: Study findings are pending at this time as our study is in-progress. Should our study demonstrate that a cognitive skills-based longitudinal wellness curriculum can lead to a measurable reduction in rates of depression, anxiety and burnout among family medicine residents, it could suggest important implications for the standardized incorporation of similar curricula into residency and continuing medical education

Lydia U Lee M.D.; Margaret Dobson, M.D.; Jill Schneiderhan, M.D.
11:15 - 11:45 AM Torrey Hills AB
L064A Advocacy: Teaching residents the professional skills necessary to change “What Is” into “What Should Be”
Most medical students often choose an altruistic path to medicine, driven by passion to improve the health and well being of patients and communities. However, often these passions become neglected due to a passive educational experience that focuses nearly exclusively on the biomedical education of disease processes, while overlooking the role that public health and health policy plays in determining wellness versus illness. Medical learners as well as practicing physicians may feel helpless when working within a system that they see as counterproductive to achieving improved health for their patients. Physicians can begin to feel empowered to improve the healthcare system as well as the health of their patients and communities by learning how public health policies shape medical care and wellness, and by choosing to engage in advocacy work. This session will describe the concept of “Advocacy as a Professional Skill”, and a unique educational program to teach these skills to residents.
11:15 AM - 12:15 PM Golden Hill B
CF3 Adolescent Champions: An Innovative Model to Optimize Health Care Delivery to Teen Patients
Adolescent patients have unique healthcare needs that may not be met by a traditional primary care practice. While they are more likely to engage in high-risk behaviors than other age ranges, adolescents access critical primary care services at lower rates than any other age groups. We aimed to develop and assess the effects of implementing the Adolescent Champion (AC) model to help primary care sites become more adolescent-centered. In the AC model, a physician partners with a health center manager and other members of the health care team to become Adolescent Champions. This interdisciplinary group undergoes trainings to learn about organizational change, quality improvement, and adolescent health issues such as confidentiality, cultural competency, and adolescent brain development. Using a train-the-trainer approach, the ACs then bring this knowledge back to their clinic highlighting key issues in adolescent health. Additionally, participating sites made youth-friendly site changes, implemented a standardized screening tool for risky behaviors, and completed a quality improvement project regarding confidentiality. Adolescent patients, staff, and providers were surveyed at baseline and year-end to assess changes.
Upon completion of this session, participants should be able to:
- Participants will be able to identify reasons for adolescent health disparities and key aspects of the AC model that aim to address these disparities.
- Recognize key factors to help primary care sites become more adolescent centered; such as multidisciplinary staff education on confidentiality laws and implementing a standardized risk assessment screening tool.
- Strategize ways to incorporate key aspects of the AC model into their own practices.
Elizabeth Shih, MD; Margaret Dobson, MD; Amy Locke, MD; Margaret Riley, MD; Allison Ursu
11:45 AM - 12:15 PM Torrey Hills AB
L064B Using Multidisciplinary Staff Training to Improve Patient-Centered Care for Transgender Adolescents
The Michigan Medicine Adolescent Health Initiative (AHI) created the award-winning Adolescent Champion model to help primary care sites optimize care for their adolescent patients. One component of the Adolescent Champion model is “sparks” – brief prepackaged,mini-trainings on adolescent health content to deliver to providers and staff. Sparks contain a script and an engaging slideshow with case scenarios, video clips, and discussion prompts. They are meant to ignite reflection, conversation, and constructive dialogue about issues important in providing adolescent-centered care. AHI created a Spark on “Patient-Centered Care for Transgender Youth,” which will be highlighted in this session, in addition to sharing transgender youth-informed experiences to illustrate affirming and respectful healthcare practices, policies and procedures to engage participants in critical reflection of their own current knowledge and attitudes while learning terminology and best practices.
Margaret Riley, M.D.; Jennifer Lane, M.A.
1:45 PM - 2:15 PM Solana Beach B
L025A Partnering with Communities to Promote Health
As we enter the era of population medicine, physicians are challenged to find ways to integrate better within our communities and to leverage already available resources to improve the health of our patients. Oftentimes, communities may have under-used resources that can help promote healthy behavior, but it may be difficult to understand how to fully utilize these connections. The University of Michigan Department of Family Medicine has been working to improve collaboration with available community resources such as the National Kidney Foundation’s Diabetes Prevention Program, as well as a local medical fitness exercise program to improve the health of patients and communities. This session will identify challenges and barriers to community collaboration as well as adopted workflows that identify appropriate patients to facilitate referrals. Data will be presented outlining tangible health outcomes achieved through these referrals.
Upon completion of this session, participants should be able to:
- Identify possible partners within the community who provide programming that would benefit the health of patients.
- Identify and adapt workflows that may augment referrals to community programming that can improve health outcomes.
- Demonstrate measurable objective improvements in health that occur when patients engage in community programming designed to improve health.
Anne Kittendorf, M.D.; Kathryn Harmes, M.D.
Monday, May 8, 2017
10:00 AM - 11:00 AM Grand AB
FP115 Primary Care Physicians’ Understanding and Referral Rates of CBT for Chronic Pain
Purpose: Chronic pain takes a heavy toll on society, and despite a wide range of available medications and physical therapies, many patients do not gain relief. The true prevalence of chronic pain is unknown, but estimates of prevalence in the United States range from 14.6 to 64%. In 2012, the National Health Interview Survey estimated that 126.1 million adults reported some pain in the previous 3 months at any one time. Cognitive behavioral therapy (CBT) is an effective adjunct to standard therapy for almost all chronic pain syndromes; yet there is little information about whether it is utilized. This study sought to investigate PCP utilization and knowledge of CBT for treating the chronic pain syndromes low back pain, fibromyalgia, and migraines. Methods: This is a cross sectional anonymous survey of primary care physicians that evaluates the prevalence of PCP utilization and understanding of CBT for chronic pain syndromes. An electronic survey was distributed in Fall 2016, to family medicine physicians in the Michigan Academy of Family Physicians and ten family medicine residency programs in Michigan. This survey included 13 questions about: 1) responder demographics, 2: knowledge questions such as CBT indications, modalities, and purpose, 3) estimated referral rates to CBT for fibromyalgia, low back pain, and migraines. Results: Eighty-six physicians responded. Data analysis is currently on-going. For the knowledge questions, each question will be assigned a point value, for a total possible score of 11 points. The results will be analyzed with SPSS to calculate the mean knowledge score and standard deviation. To estimate prevalence of CBT referrals, we will calculate the proportion and corresponding 95% confidence interval of providers who refer patients to CBT within each of the pain condition. Multivariable logistic regression will be used to assess adjusted relationships between provider demographics, knowledge scores, and likelihood of referral to CBT. Conclusions (Anticipated): This data will help us gain better understanding about PCPs’ comprehension and utilization of CBT for treating chronic pain, specifically fibromyalgia, low back pain, and migraines. If the conclusion is consistent with our hypothesis that referral rates are low, we may use this data to educate primary care physicians about the effectiveness of CBT for chronic pain, as well as spread awareness of the underutilization of CBT.
Yujing Lin, M.D.; Melissa Plegue, MA; Jill Schneiderhan, M.D.; Ananda Sen, Ph.D.; Suzanna Zick, N.D., M.P.H.
FP119 Assessment of Knowledge, Attitudes and Behaviors about Palliative and End of Life Care amongst Resident Physicians
Purpose: Resident physicians are frequently involved in providing palliative care as part of their training, yet there is sparse data comparing competency in palliative care between specialties. This study aims to compare self-perceived competencies in various domains of end of life care by resident specialty. Methods: Sixty-one residents spanning three different specialties (Family Medicine, Internal Medicine and Medicine/Pediatrics) at the University of Michigan Health System were electronically surveyed between September – December 2015 using the End-of-Life Questionnaire (EOLC-Q) developed by Montagnini, Smith and Balistrieri (2012). The survey consists of 28 specific questions and 4 open-ended questions examining self-perceived knowledge, attitudes and behaviors regarding the provision of palliative and end of life care in the hospitalized patient. Multivariate Analysis of Variance (MANOVA) was used to analyze quantitative data. Results: A total of 61 residents participated (response rate 29%). Differences were observed between the three specialties among the various scale scores. Residents from Family Medicine and Internal Medicine scored higher than their colleagues in Medicine/Pediatrics in knowledge, behavior, decision-making, communication and symptom management (p<0.005). There were no significant differences among specialties in attitude, continuity of care, emotional and spiritual support for patients and families. Conclusions: Residents in Family Medicine and Internal Medicine report higher self-perceived competency in certain areas of palliative care when compared to their colleagues in Medicine/Pediatrics, yet more research is needed examining what factors may explain these self-reported differences and whether they translate into differences in quality of care. This study has important implications for resident physician training and may help guide the development of interventions aimed at addressing differences in self-perceived competencies among these specialties.
Justin Oldfield, M.D.; Tyler Policht M.D.; Thomas A O'Neil, M.D.; Bidisha Ghosh M.S.; Marcos Montagnini M.D., F.A.C.P.
FP136 Evaluation of resident sense of preparedness in performing hand-off on an inpatient medicine service before and after implementation of the IPASS hand-off tool
Purpose: Unstructured hand-off in the inpatient setting is known to result in communication of incorrect or incomplete patient data, which in turn increases the number of preventable medical errors. Often, residents are not adequately trained on how to perform proper written and verbal hand-off. The goal of this study is to evaluate resident attitudes with respect to preparedness and efficiency before and after implementation of the IPASS hand-off tool, and to provide formal feedback on their performance. Methods: Thirty-three family medicine residents (HO1-HO3) will be surveyed on their hand-off practices prior to implementation of a structured tool for verbal and written hand-off. At the start of their inpatient medicine month at a local community hospital, residents will undergo a 1-hour abbreviated IPASS training session in which they will learn and practice the essential components of effective verbal and written hand-off. Residents will be evaluated one week and four weeks into their inpatient rotation using the IPASS faculty evaluation tool. The evaluation performed at one week will provide formative feedback to the resident, and the repeat evaluation at four weeks will assess the development of hand-off skills over the course of the rotation. Finally, a post-implementation survey will be completed to evaluate resident attitudes toward use of the IPASS hand-off tool versus unstructured hand-off, including perceived effects on preparedness and efficiency. Results: This study is ongoing. Results will help to better characterize resident attitudes toward a formal hand-off process versus a previously unstructured model. In addition, it will allow for evaluation of skills after targeted training on how to effectively perform verbal and written hand-off, which is not currently a formal part of the curriculum. Conclusions: Pending completion of the study. It is anticipated that implementation of the IPASS hand-off tool, while labor intensive initially, will result in greater efficiency and resident sense of preparedness in performing verbal and written hand-offs, as well as provide a forum for formal feedback on performance of these skills.

Kristine L Cece, M.D., Ph.D.; Patricia Mullan, Ph.D.
Tuesday, May 9, 2017
8:00 AM - 9:30 AM
W15 Writing for Publication: What Works and What Doesn't
Want to be successful at publishing your scholarly work? This session will be led by the editors of FP Essentials, the monthly monograph program that is one of American Academy of Family Physician’s largest continuing medical education programs. We will cover approaches to writing papers, editorials, letters to the editor, book chapters, monographs, and abstracts, and successfully seeing them through to publication. We will go over the various types and formats of publications, how to match your content to the publication, and will show examples of common errors made by authors. You will then join the editors in small groups to work on developing your own writing plan. Feel free to bring samples of your work for feedback and helpful comments. Opportunities will be provided to ask questions and share successes and difficulties. We will end the session with tips for authors whose papers were rejected or who are having difficulty finding time to write.
Upon completion of this session, participants should be able to:
- Identify writing opportunities, generate a topic to write about, assure sufficient knowledge of the topic, and develop a content outline and writing plan that will enhance the likelihood that the piece of writing will be published.
- Choose the appropriate publication (i.e., journal, book, monograph, etc) for the planned piece of writing.
- Address the various steps in the writing, review, revision, and publication processes. If a manuscript or proposal is rejected, assess the reasons why, revise appropriately, and submit to another publication.
Barry Weiss, M.D.; Karl Rew, M.D.; Kathleen Rowland, M.D., MS; Mindy Smith, M.D., M.S.
Virtual Poster Session
A publication based on this research, entitled "Real-time data collection using text messaging in a primary care clinic" is forthcoming in the journal Telemedicine and e-Health.